To support Victorian government effort to curtail the spread of coronavirus, Geelong Chinese Medicine Clinic will open to provide essential service to our patients during the circuit-breaker lockdown. During this period, our staff might wear a face shield, in addition to a mask. This is to protect you, and the community. Thank you for your understanding.
Geelong Chinese Medicine Clinic wishes you well and safe. Remember to be gentle to yourself and to your family.
To support Victorian government effort to curtail the spread of coronavirus, Geelong Chinese Medicine Clinic will temporarily suspend practice from Friday 28 May to Thursday 3 June. The clinic will resume to practice on Friday 4 June to provide essential service to our patients.
We continue with our strict hygiene protocol and our preventative measures:
Meanwhile please check our blog on 10 Tips to avoid impact of coldness when work from home.
Geelong Chinese Medicine Clinic wishes you well and safe. Remember to be gentle to yourself and to your family.
Geelong Chinese Medicine Clinic (GCMC) wishes everyone a very Happy New Year! 2020 has been a challenging year to everyone. Looking back, we should be so proud of ourselves for our resilience and our kindness to each other.
“Every end marks a new beginning”. 2021 will be a new chapter. Each of us has a pen in our hand to write a few beautiful stories for ourselves.
In 2021, GCMC will continue to serve you and work with you to build inner strength, and bring out peace and the beautiful stories in you.
With the recent changes in the restrictions as outlined by the state government, Geelong Chinese Medicine has updated its operation. As of 28 September 2020,
We continue with our strict hygiene protocol and our preventative measures:
During this special time, please check our regular “Blogs” for free advice on selfcare.
Geelong Chinese Medicine Clinic wishes you well and safe. Remember to be gentle to yourself and to your family.
To support Victorian government effort to curtail the spread of coronavirus, Geelong Chinese Medicine Clinic will temporarily stop taking new patients, and will continue to serve existing patients via adjusted methods from 4 August 2020. We will re-assess the situation week by week.
During this difficult time, please check our regular “Blogs” for free advice on selfcare.
Let us work together to combat the pandemic.
Geelong Chinese Medicine Clinic wishes you well and safe during this difficult time. Remember to be gentle to yourself and to your family.
In responding to the 2nd spike of COVID-19, Geelong Chinese Medicine Clinic is adopting more strict preventative measures, in addition to our existing infection control procedure and social distancing policy (Please see entry of 1 May 2020).
Stay safe, and stay well. Let us work through this time together.
Geelong Chinese Medicine is now resuming its operation from 1st of May 2020.
Here are some procedures we have in place to keep everyone safe during COVID-19 time.
All practitioners at Geelong Chinese Medicine Clinic underwent further training about infection control associated with COVID-19. We adopt strict infection control procedures in our clinic.
We provide sanitisers for patients to sanitise their hands prior to entering the treatment room and when they leave the room.
Lifeline: 13 11 14
Beyond Blue: 1300 22 4636
Coronavirus Health Information Line: 1800 020 080
To support government effort to curtail the spread of coronavirus, we will temporarily suspend face to face consultation and acupuncture service from Mon 30th March. We will re-assess the situation week by week.
Let us work together to combat the pandemic.
Geelong Chinese Medicine Clinic wishes you well and safe during this difficult time. Remember to be gentle to yourself and to your family.
For 20 years, Geelong Chinese Medicine Clinic – GCMC – has being providing acupuncture and Chinese herbal medicine to the community of Geelong, the Surf Coast and surrounding areas from the headquarters of the Corio Bay Health Group.
Our logo is an ancient symbol, representing peace, greatness and harmony. It has the symbol of Yang under and Yin above, indicating the inner strength and outward gentleness, to achieve resilience and peace.
At the Geelong Chinese Medicine Clinic, we are passionate about, and work towards, relieving your suffering, building your inner strength and bringing out peace. All of our practitioners have dual registration of acupuncture and Chinese herbal medicine with Australian Health Practitioner Registration Agency (AHPRA). We are highly qualified and experienced practitioners.
We use traditional as well as modern acupuncture, such as laser acupuncture, electrical acupuncture and needle-free acupuncture. We often combine Chinese herbal medicine and acupuncture.
Chinese Medicine understands that good health relies on the restoration and maintenance of normal function, and focuses on the prevention of illness as well as treatment. We use acupuncture, Chinese herbal medicine, and Chinese medicine wisdom to improve your symptoms and address the causes.
The commonest conditions that we treat and produce effective results are:
We use Chinese medicine principles and theories to diagnose and treat a wide range conditions, including
For a further listing of conditions commonly treated by Chinese medicine, including acupuncture and Chinese herbal medicine, please see lists the AACMA official website (click on the links below).
Conditions suitable for acupuncture treatment
Conditions suitable for Chinese herbal medicine treatments
At Geelong Chinese Medicine Clinic, we see each person as an individual because each of us has different constitutions and past history. We develop personalised treatment plans for each person to achieve the long-term result.
Putting you at the centre of our practice, at Geelong Chinese Medicine Clinic we take a holistic approach to your health and well-being, with services to boost your mind-spirit-body connection for optimum function, happiness, peace and clarity of mind.
As well as traditional acupuncture, our Chinese medicine practitioners are skilled in laser acupuncture, electroacupuncture and other non-invasive treatments, such as cupping, moxibustion and the art of Qigong.
All of us hold high-level professional qualifications and a wealth of clinical experience in Australia. We hold dual registration of acupuncture and Chinese herbal medicine with Australian Health Practitioner Regulation Agency (AHPRA).

At Geelong Chinese Medicine Centre, we provide all information our patients need to know before their treatment, including acupuncture insurance cover and what to expect when you make your appointment with us.
Geelong中医诊所在过去近二十年中以高尚的医德和精湛的技术,衷心为Geelong人民竭诚服务。
医资力量
诊所的三位医生都是澳大利亚注册的中医师。
郑真医生系世界著名的南京中医药大学的毕业生,有二十多年的临床经验,墨尔本大学的博士,皇家理工大学(RMIT)副教授,擅长將中医和现代医学知识结合以治疗各类疼痛及其他常见病。
Lauren张医生系世界著名的南京中医药大学的医学硕士,有十几年的临床经验,擅长治疗女性疾病和不孕症.
郑真医生和Lauren张医生都能够用流利的英文和华语(普通话 )与患者沟通。
服务理念
Geelong中医诊所以患者为第一。 用中药、针灸、拔罐、耳针等中医传统方法为大众服务,治疗结束后还会传授患者在家用中医养身和膳食调理,以便巩固和提高治疗效果。
地理位置
Geelong中医诊所位于Geelong中心的一家大型西人理疗中心中,我们与西医医生、理疗师及其他职业医师有着密切的合作关系以为患者提高疗效。
Free parking is available at the Geelong Chinese Medicine Clinic.
Bob, F., & Philippe, S. (2001) The Treatment of Modern Western Medical Diseases with Chinese Medicine. Boulder, CO: Blue Poppy Press.
Will, M., & Jane, L. (2008) Clinical Handbook of Internal Medicine – The treatment of Disease with Traditional Chinese Medicine. Sydney: University of Western Sydney.
Chirali,. I. (2007). Traditional Chinese Medicine Cupping Therapy (2nd ed.) Philadelphia, PA: Elsevier.
Cao, H., Han, M., Li, X., Dong, S., Shang, Y., Wang, Q., … Liu, J. (2010). Clinical research evidence of cupping therapy in China: a systematic literature review. BMC Complementary and Alternative Medicine, 10(1). doi:10.1186/1472-6882-10-70
Cao, H., Li, X., & Liu, J. (2012). An updated review of the efficacy of cupping therapy. PLoS One, 7(2), doi: 10.1371/journal.pone.0031793.
Dharmananda, S. (1999). Cupping.
http://www.itmonline.org/arts/cupping.htm (Accessed 01 Sep 2018)
Mehta, P., & Dhapte, V. (2015). Cupping therapy: A prudent remedy for a plethora of medical ailments. Journal of Traditional and Complementary Medicine, 5(3), 127–134. http://doi.org/10.1016/j.jtcme.2014.11.036
Maciocia, G. (1989). The foundations of Chinese medicine: A comprehensive text for acupuncturists and herbalists. Edinburgh: Churchill Livingstone.
Guo, B., & Powell, A. (2002). Listen to Your Body: The Wisdom of the Dao. Honolulu: University of Hawai’i Press.
Painaustralia (n.d), Fact sheet 1-The Nature and Science of Pain [Online] Available from: http://painaustralia.staging3.webforcefive.com.au/static/uploads/files/painaust-factsheet1-wftffeqmvcqm.pdf [Accessed 8 Aug 2018].
MayoClinic (2016),Understanding Pain, 2016 [Online] Available from: https://www.mayoclinic.org/understanding-pain/art-20208632 [Accessed 8 Aug 2018].
Russell, D. & Hopper Koppelman, M. (2017). Acupuncture For Pain. Evidence Based Acupuncture. Available from: https://www.evidencebasedacupuncture.org/present-research/pain-2/#foot_loc_16603_18 [Accessed 8 Aug 2018].
Xiang, A., Cheng, K., Shen, X., Xu, P., & Liu, S. (2017). The Immediate Analgesic Effect of Acupuncture for Pain: A Systematic Review and Meta-Analysis. Evidence-Based Complementary and Alternative Medicine : eCAM, 2017, 3837194. http://doi.org/10.1155/2017/3837194
Weidenhammer W, Streng A, Linde K, Hoppe A, Melchart D. Acupuncture for chronic pain within the research program of 10 German Health Insurance Funds–basic results from an observational study. Complementary therapies in medicine. 2007;15(4):238-46.
American Specialty Health Incorporated Health Services Department. (2016). Acupuncture: Does Acupuncture Provided Within a Managed Care Setting Meet Patient Expectations and Quality Outcomes?, 1–12. http://files.clickdimensions.com/ashcompaniescom-a7oce/files/acupuncturecahps.pdf
Yin, C., Buchheit, T. E., & Park, J. J. (2017). Acupuncture for chronic pain: an update and critical overview. Current Opinion in Anaesthesiology, 1. https://doi.org/10.1097/ACO.0000000000000501
H. Y. Chiu, Y. J. Hsieh, and P. S. Tsai, “Systematic review and meta-analysis of acupuncture to reduce cancer-related pain,” European Journal of Cancer Care, vol. 26, no. 2, Article ID e12457, 2017.
C. H. Y. Lau, X. Wu, and V. C. H. Chung, “Acupuncture and Related Therapies for Symptom Management in Palliative Cancer Care: systematic Review and Meta-Analysis,” Medicine (Baltimore), vol. 95, no. 20, Article ID e90e6, p. e2901, 2016.
Z. Lu, H. Dong, Q. Wang, and L. Xiong, “Perioperative acupuncture modulation: More than anaesthesia,” British Journal of Anaesthesia, vol. 115, no. 2, pp. 183–193, 2015.
Flaws, B. (2000). Curing Fibromyalgia Naturally With Chinese Medicine. Colorado. Blue Poppy Press.
Maciocia, G. (1989). The foundations of Chinese medicine: A comprehensive text for acupuncturists and herbalists. Edinburgh: Churchill Livingstone.
Chang, S., & Wang, H. (2004). Health promotion in traditional Chinese medicine: preventive treatment of a disease. Hu Li Za Zhi, 51(2), 23-7. Review. Chinese. PubMed PMID: 15137181.
Bian, L., Liu, Z., & Li, G. (2015). Promoting health wellness—The essentials of Chinese medicine. Chinese Journal of Integrative Medicine, 21(8), 563. https://doi.org/10.1007/s11655-015-2100-y
Koithan, M., & Wright, C. (2010). Promoting Optimal Health with Traditional Chinese Medicine. The Journal for Nurse Practitioners : JNP, 6(4), 306–307. http://doi.org/10.1016/j.nurpra.2010.01.013
Chen, L., & Su, Y. (2007). Health promotion for deficient constitution in Chinese medicine. Hu Li Za Zhi, 54(4), 16-20. Chinese. PubMed PMID: 17654423.
Zeng Y, Luo T, Xie H, Huang M, Cheng A. (2014). Health benefits of Qigong or Tai Chi for cancer patients: a systematic review and meta-analyses. Complement Ther Med, 22,173–186.
https://doi.org/10.1016/j.ctim.2013.11.010
Tai Chi Australia (2017), What is Qigong? [Online] Available from:
http://www.taichiaustralia.com.au/Qigong/what-is-qigong [Accessed 13 Aug 2018].
Jahnke, R., Larkey, L., Rogers, C., Etnier, J., & Lin, F. (2010). A Comprehensive Review of Health Benefits of Qigong and Tai Chi. American Journal of Health Promotion : AJHP, 24(6):1–25. http://doi.org/10.4278/ajhp.081013-LIT-248
Sancier, K. M., & Holman, D. (2004). Multifaceted health benefits of medical Qigong. Journal of Alternative and Complementary Medicine: JACM, 10(1):63–166. http://doi.org/10.1089/107555304322849084
Xiangcai, X. (2000). Qigong for treating common ailments: the essential guide to self-healing. (2nd ed.). Boston, MA: YMAA Publication Center.
Yang, J.M., (2008). A Brief History of Qigong. [Online] Available from: http://legacy.ymaa.com/articles/history/history-qigong. [Accessed 13 Aug 2018].
Yang, J.M., (2013). What is Taijiquan? [Online] Available from: http://legacy.ymaa.com/articles/2013/05/what-is-taijiquan [Accessed 13 Aug 2018].
Ladawan S., Klarod K., Philippe M., Menz V., Versen I., Gatterer H., Burtscher M. (2017), Effect of Qigong exercise on cognitive function, blood pressure and cardiorespiratory fitness in healthy middle-aged subjects. Complement. Ther. Med.33:39–45. https://doi.org/10.1016/j.ctim.2017.05.005
Zou, L., SasaKi, J. E., Wang, H., Xiao, Z., Fang, Q., & Zhang, M. (2017). A Systematic Review and Meta-Analysis Baduanjin Qigong for Health Benefits: Randomized Controlled Trials. Evidence-Based Complementary and Alternative Medicine : eCAM. http://doi.org/10.1155/2017/4548706
Yang, H., Wu, X., & Wang, M. (2017). The Effect of Three Different Meditation Exercises on Hypertension: A Network Meta-Analysis. Evidence-Based Complementary and Alternative Medicine : eCAM. http://doi.org/10.1155/2017/9784271
Cheung, B.M., Lo, J.L., Fong, D.Y., Chan, M.Y., Wong, S.H., Wong, V.C., Lam, K.S., Lau, C.P., Karlberg, J.P. (2005), Randomised controlled trial of qigong in the treatment of mild essential hypertension. Journal of Human Hypertension.19(9):697–704. https://doi.org/10.1038/sj.jhh.1001884
Lomas-Vega, R., Obrero-Gaitán, E., Molina-Ortega, F.J., Del-Pino-Casado, R. (2017), Tai chi for risk of falls. A meta-analysis. J Am Geriatr Soc.65(9):2037-43.https://doi.org/10.1111/jgs.15008
Tsang, H. W., Fung, K. M., Chan, A. S., Lee, G. and Chan, F. (2006), Effect of a qigong exercise programme on elderly with depression. Int. J. Geriat. Psychiatry, 21:890-897. doi:10.1002/gps.1582.
Li, F., Fisher, K.J., Harmer, P. , Irbe, D. , Tearse, R.G. and Weimer, C. (2004), Tai Chi and Self‐Rated Quality of Sleep and Daytime Sleepiness in Older Adults: A Randomized Controlled Trial. Journal of the American Geriatrics Society, 52:892-900. https://doi.org/10.1111/j.1532-5415.2004.52255.x
Fransen, M., Nairn, L., Winstanley, J., Lam, P. and Edmonds, J. (2007), Physical activity for osteoarthritis management: A randomized controlled clinical trial evaluating hydrotherapy or Tai Chi classes. Arthritis & Rheumatism, 57:407-414. doi:10.1002/art.22621
Chan, Kaiming et al. (2004), A randomized, prospective study of the effects of Tai Chi Chun exercise on bone mineral density in postmenopausal women
Arch Phys Med Rehabil, 85(5):717-22.
https://doi.org/10.1016/j.apmr.2003.08.091
Hamasaki, H. (2017), Exercise and gut microbiota: clinical implications for the feasibility of Tai Chi. J Integr Med.15(4):270–281.
https://doi.org/10.1016/S2095-4964(17)60342-X
Klein, P. (2017). Qigong in Cancer Care: Theory, Evidence-Base, and Practice. Medicines, 4(1),2. http://doi.org/10.3390/medicines4010002
Wang, C., Roubenoff, R., Lau, J., Kalish, R., Schmid, C.H., Tighiouart, H., Rones, R., Hibberd, P.L.(2005), Effect of Tai Chi in adults with rheumatoid arthritis, Rheumatology, 44(5):685–687. https://doi.org/10.1093/rheumatology/keh572
Ladawan, S., Klarod, K., Philippe, M., Menz, V., Versen, I., Gatterer, H., Burtscher, M. (2017), Effect of Qigong exercise on cognitive function, blood pressure and cardiorespiratory fitness in healthy middle-aged subjects. Complement Ther Med.33:39-45. doi: 10.1016/j.ctim.2017.05.005.
Wayne, P.M., Walsh, J.N., Taylor-Piliae, R.E., Wells, R.E., Papp, K.V., Donovan, N.J., & Yeh, G.Y. (2014). The Impact of Tai Chi on Cognitive Performance in Older Adults: A Systematic Review and Meta-Analysis. Journal of the American Geriatrics Society, 62(1):25–39. http://doi.org/10.1111/jgs.12611
Lauche, R., Langhorst, J., Dobos, G., Cramer, H. (2013), A systematic review and meta-analysis of Tai Chi for osteoarthritis of the knee. Complement Ther Med.21(4):396-406. https://doi.org/10.1016/j.ctim.2013.06.001
Wang, C., Schmid, C. H., Iversen, M. D., Harvey, W. F., Fielding, R. A., Driban, J. B., … McAlindon, T. (2016). Comparative Effectiveness of Tai Chi Versus Physical Therapy for Knee Osteoarthritis: A Randomized Trial. Annals of Internal Medicine, 165(2):77–86. http://doi.org/10.7326/M15-2143
Zheng, G., Li, S., Huang, M., Liu, F., Tao, J., & Chen, L. (2015). The Effect of Tai Chi Training on Cardiorespiratory Fitness in Healthy Adults: A Systematic Review and Meta-Analysis. PLoS ONE,10(2). http://doi.org/10.1371/journal.pone.0117360
Ann Pietrangelo and Stephanie Watson, “11 Effects of Sleep Deprivation on Your Body”. Available from https://www.healthline.com/health/sleep-deprivation/effects-on-body [Accessed 3 Sep 2018].
Thank you for contacting Geelong Chinese Medicine Clinic, we will be in touch with you as soon as possible.
Ella (Yongqi) Zhang
Qualifications: B.Science ANU, B.HlthSc & B. AppSc (ChinMed) RMIT
Pain is a distressing sensory and emotional experience associated with actual or potential tissue damage. Pain is your body’s way of alerting you to danger and letting you know what’s happening in your body. You perceive pain through sensory nerve cells. How you feel and react to pain depends on what’s causing it, as well as many personal factors. People seeking pain treatments and those seeking acupuncture and Chinese stress medicines from our Geelong clinic make up a large proportion of our patients.
While usually pain is not a condition in itself, but rather an indication/symptom of a problem somewhere in the body, if dysfunctional it can become a disease in its own right.
Pain is the most common reason that people seek medical help and can come in many forms. Usually, the location of the pain within the body corresponds with the location of the problem it is indicating, however, cases in which pain is experienced in a location away from the problem also exist, i.e. leg pain resulting from a prolapsed disk pushing on a nerve in the back. Pain can affect any part of your body.
Some of the most common forms of pain are:
There are two major categories of pain. Pain can be short-term (acute) or long-term (chronic).
Acute pain is pain lasting less than three months and occurs following surgery or trauma or other conditions. One third of people do not know what causes their pain. Although it usually improves as the body heals, in some cases, it may not.
Chronic pain is pain that lasts beyond three months, the time needed for issues to heal following surgery or trauma or other conditions. It is often associated with an increased pain experience, which may spread beyond the area of injury into surrounding tissue or nerves. It can also exist without a clear reason at all.
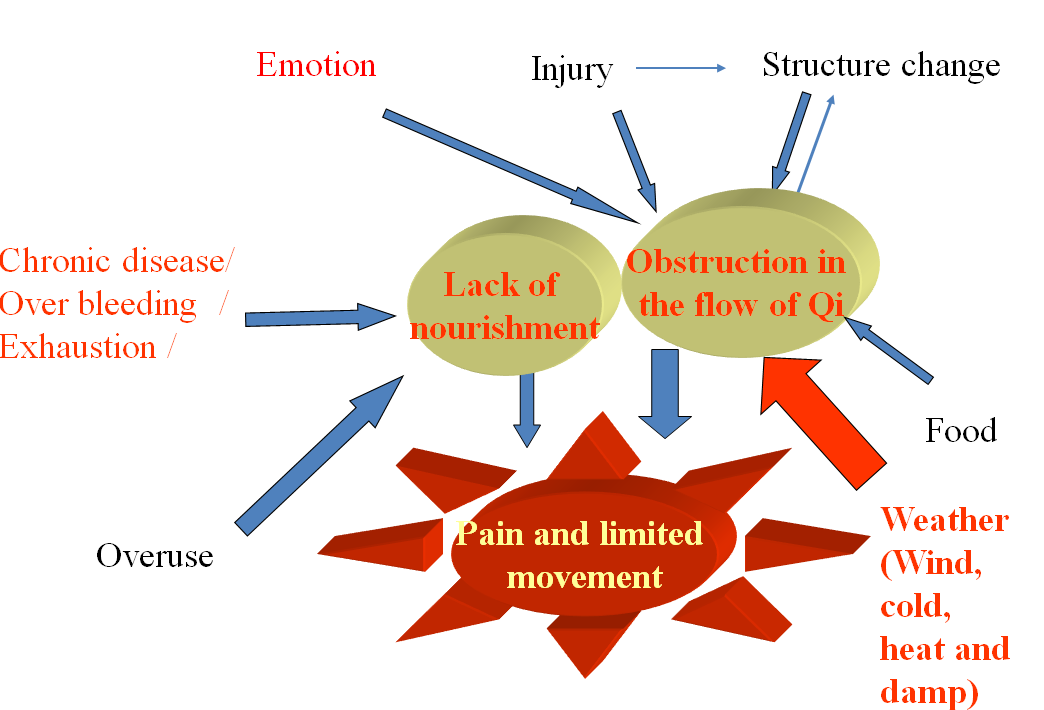
The following simple yet profound statement sums up the very essence of the Chinese medical view of pain:
This means that, as long as qi (vital energy) and blood circulate freely and smoothly without hindrance or obstruction, there is no pain in the body. However, if, due to any reason, the flow of qi and blood is hindered, blocked, obstructed, or insufficient flow, then there will be pain.
There are two main causes of the lack of free flow of the qi and blood, either:
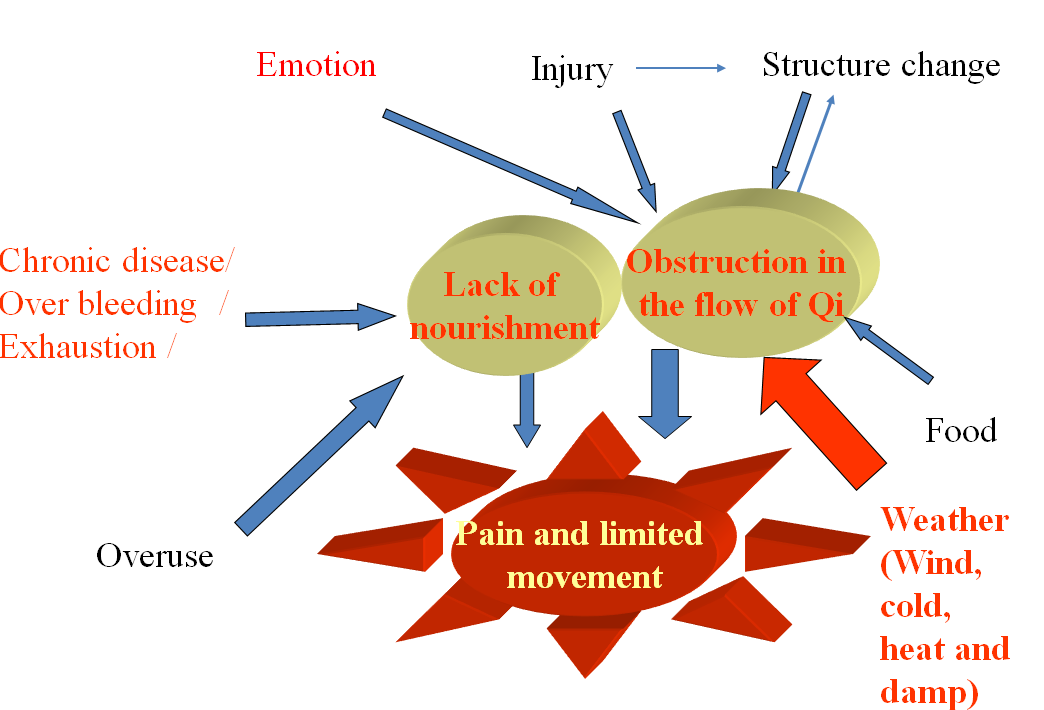
All pain, no matter what its modern Western medical diagnosis, is considered by Chinese medicine as a problem with free flow of qi and blood.
The flow of qi and blood can become inhibited in any and every area of the body: the internal organs, the muscles, the head, the lower back, and the extremities and joints.
Thus, in Chinese medicine, pain is the felt experience of the inability of the body to keep up with the maintenance of the body, be this supplying adequate nutrition/energy, regeneration of injured body parts/organs, replenishing vital cellular products, toxin processing and waste removal to maintain proper operation of the body.
In Chinese medicine, all pain disturbs the mind. This explains why people with pain often suffer from anxiety, depression and / or poor sleep.
The basic principle of treatment in Chinese medicine is to first calm the mind, then restore the flow of Qi.
In Chinese medicine, two patients with the same Western medical disease may receive radically different Chinese medicine treatment because the root cause of their disease is different. This means that every patient in Chinese medicine is given an individualised treatment based on the cause and nature of their particular pattern of disharmony.
We will identify the pattern from Chinese medicine, contributing factors, such as sleep, anxiety, and develop a treatment plan incorporating acupuncture, auricular acupressure and/or herbal medicine. We will also advise you on self-management approaches so that you could help yourself in improving pain. We communicate with other health professionals who also help you so that you have a supporting network.
There is considerable evidence of acupuncture for acute and chronic pain.
For acute pain, a 2017 systematic review found that acupuncture was more effective than both sham needling and injection with painkillers.
For chronic pain, in 2007 the largest study of its kind to date, 454,920 patients were treated with acupuncture for headache, low back pain, and/or osteoarthritis. Effectiveness was rated as marked or moderate in 76% of cases.
In a two-year retroactive survey published in 2016 of over 89,000 patients, 93% of patients said that their acupuncturist had been successful in treating their musculoskeletal pain.
Another 2017 study paper titled ‘Acupuncture for Chronic Pain: an Update and Critical Overview’ concluded that “mounting evidence supports the effectiveness of acupuncture to treat chronic low back, neck, shoulder, and knee pain, as well as headaches. Also, additional data emerging supports the use of acupuncture as an adjunct or alternative to opioids, and in perioperative settings.
Two recent 2016, 2017 systematic reviews reported positive results of acupuncture in the relief of cancer-related pain. A 2015 systematic review and meta-analysis suggested that acupuncture was useful in decreasing postoperative pain.
Please also check out Dr Zhen Zheng’s research on acupuncture for:
Geelong Chinese Medical Clinic provides a wide range of health treatments including help with sleep problems, digestion issues and allergies and also provides Chinese women’s health and fertility medicines for Geelong and district women
Stress is a common phenomenon with life. Emotional disturbance is our common reaction to stress. Chinese medicine understands emotions are one of the leading causes of health issues and diseases and our practitioners provide a variety of treatments for stress and emotional issues, including Chinese medicine in Geelong for women’s health and fertility problems.
Some causes of diseases, such as weather change, flu virus or food poisoning for example, can be avoided by taking preventative measures and keeping away from those causes. Emotion, however, is with you and within you 24/7, and it directly impacts on your body function. You might notice that your head hurts when you face a conflicting situation; you have shortness of breath when feeling sad; you have poor appetite or loss of sleep when you are worried about something. Those physical discomforts explain the close integration between body and mind and emotion.
Similarly, a dysfunctional body could also evoke an emotional response. Pain could lead to depression and poor sleep is often associated with anxiety, which is why the Chinese medicine and treatment for sleep problems at our Geelong clinic incorporates a holistic all-of-body approach.
Chinese medicine sees the body and mind as one, inseparable, and that each affects the other. The symbiosis between body and mind is integral to how we approach the treatment of emotional issues and stress at Geelong Chinese Medicine Clinic.
Because of the close interaction between mind and body, Chinese medicine treats both the body and mind to address stress and emotional issues.
We will treat the impact of emotions on your body as well as calm your mind to produce therapeutic effects. We will work with other health practitioners, such as your psychologist, psychiatrist or GP, to help you. The ultimate goal is to help you regain the sense of peace and wellbeing to produce long-term results.
Based on Chinese medicine diagnosis, our practitioners in Geelong use acupuncture treatments to:
Chinese herbal medicine is also used to strengthen the results. We will provide “take home” treatments so that you can continue with the treatment effects and gain some sense of control. We will also provide advice on lifestyle changes to enable you to self-manage for long-term results.
Please contact our clinic for a range of Chinese medicine treatments, including resolving sleep problems and women’s health and fertility treatments in Geelong.
A woman’s body goes through delicate changes throughout its lifetime, from the onset of first menstrual period to menopause and our clinic places strong emphasis on the provision of Chinese women’s health and fertility medicine for Geelong and district women. From Chinese medicine’s point of view, women’s reproduction relies on kidney “Jing” or essence, as well as coordinated organs functioning. We also believe women’s physiology is dominated by blood.
In women, blood is not only the source of periods but also of fertility, conception, pregnancy, childbirth and breastfeeding. Menstruation period is an indicator of women’s general health. It is very important that menstruation is punctuated with moderate amount of blood as it reflects good Qi (energy) and blood circulation.
Unhealthy lifestyle, diet and stress can all play a big role in changing women’s dynamic balance, causing symptoms physically and mentally. Most women had those episodes when their periods were delayed or stopped for one or more months after an emotionally or physically stressful time.
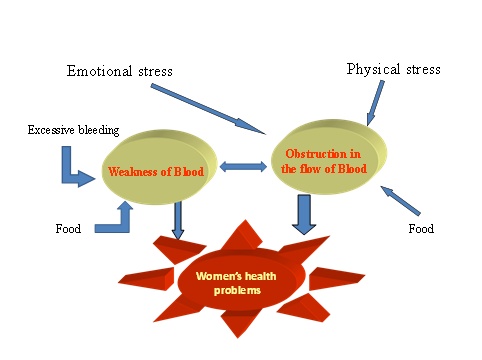
We usually combine Chinese herbal medicine and acupuncture at our Geelong clinic to treat women’s health problems. Diet and lifestyle change are also provided. We treat body and mind as one during treatment as they cannot be separated.
Regulating period circles is our priority. For fertility issues, a good period circle reflects balanced hormonal levels and it also leads to proper timing of ovulation. Generally, a long menstruation circle associates with a delayed ovulation, and a short circle comes with an earlier ovulation.
Eliminating associated symptoms is also very important. Our goal is to get you through circles without much pain and suffering.
Geelong Chinese Medicine Clinic provides a range of treatments and Chinese herbal medicines in Geelong, including cupping and moxibustion, needle-free acupuncture, treatments for digestion issues and Chinese medicine and treatments for sleep problems.
The following symptoms can be a sign you do not sleep well or are suffering from a lack of sleep:
Sleep is closely related to main parts of our lives. In the long-term, sleep deprivation can have a serious impact on mental acuity and physical health. Poor sleep is linked with many health problems, including diabetes, high blood pressure, heart disease risk, weight gain and generally weakened immunity.
If you have experienced any of the above symptoms, consult Geelong Chinese Medicine Clinic about different natural approaches to improve sleeping and to discuss our range of preventative Chinese medicine for Geelong and district patients.
In Chinese medicine, sleep is a representation of balanced yin and yang, and a calm mind. One can only fall asleep at night if they are generally calm in their mind during the day and prior to sleep.
More than 50 percent of patients we see at the Geelong Chinese Medicine Clinic experience some sleeping problems, but only 20 percent come specifically to have treatment for sleep.
There are multiple causes responsible for sleep problems, including:
Sleep hygiene is a must for a good sleep. To learn about sleep hygiene, please check this site from the Victorian Government.
Contact our clinic to discuss a range of traditional Chinese medicines and treatments including needle-free acupuncture, Qi Gong, help with women’s health and fertility problems, help with stress and emotional issues and our Chinese herbal medicines in Geelong.
While in general modern people think of healthcare and medicine as something for when you are unwell, traditional Chinese medicine (TCM) is a medicine that holds “prevention is better than cure and health promotion is the best method for prolonging one’s own life”.
TCM views health as the balanced condition of a person’s mind, body and spirit, usually meaning to be free from illness, stress, injury or pain.
So in TCM, health is ‘life in balance’. This is demonstrated in the Daoist concept of yin and yang, represented by the tai ji or yin yang symbol.
Explaining the TCM value of health promotion and disease prevention methods is like comparing the human body to a car engine – it has specific functions that require regular maintenance, care and attention. In the TCM view, vital energy (Qi) flows throughout the body and when it gets blocked or becomes stagnant, health issues can arise.
Receiving regular, or semi-regular TCM treatments and following TCM principles helps provide the necessary support the body needs to stay at optimum operating levels. This also aims to address any issues before they become a bigger problem.
According to TCM theory, disease can be caused by a combination of:
The body’s ability to respond to these disturbances relies on a balanced and healthy capacity. If a person suffers any amount of these disorders over time, eventually it will lead to a disturbance or imbalance of Qi, which compromise the body-mind-spirit of the person and leaves them open to disease.
However the body’s warning system is to exhibit symptoms which signal that it has somehow fallen out of balance. These start as vague discomforts and intermittent low-level symptoms, such as:
These symptoms may increase in intensity and eventually become an identifiable illness if ignored.
In TCM, good health is quite similar to what your mother has been telling you for as long as you can remember! Harmony and balance in every aspect of life is the key to health.
Where the body’s balance is showing signs of being disturbed, the main goal of TCM is to restore balance by influencing the many forms of the body’s Qi using direct and indirect methods reflecting TCM theories, including:
If identified and treated early, imbalances are much more easily restored than long-standing issues. Please contact our clinic for more information, treatments and Chinese herbal medicines in Geelong.
In Chinese medicine, good gut health and digestion contributes to overall good health, contentment, hardiness and happiness. While good digestion aids optimum body function, digestion problems can lead to a range of health concerns, as well as affecting everyday life and leading to feelings of melancholy.
If you frequently suffer from stomach aches, bowel troubles or find that certain foods cause indigestion, we at Geelong Chinese Medicine Clinic can help identify the underlying cause and provide natural remedies. The Chinese acupuncture and Chinese herbal medicines at our Geelong clinic can help relieve symptoms of poor digestion and boost digestive function.
Traditional Chinese medicine takes a holistic approach to treating digestive problems, looking closely at the way your digestive network functions.
If there is an imbalance or issue in any one of your organs, the entire network becomes disrupted.
A Chinese medicine practitioner knows how to find the issue. There are common signs that suggest poor digestive health, including:
Poor nail health can indicate an inability to absorb and digest nutrients from food.
The appearance of different sections of the tongue is directly linked to organs in the digestive network. The colour, shape and size of the tongue can tell a Chinese medicine practitioner important information about the function of particular organs, while ulcerations, coatings on the tongue and visibility of blood vessels can reveal information about digestion and absorption in the digestive tract, as well as indicate food intolerances.
In Chinese medicine, a healthy and balanced diet is vital for good gut health – and promotes overall well-being, optimism and clarity. Over-eating, under-eating or eating foods with low nutritional value leads to Qi Stagnation and Food Accumulation and feelings of hunger or discomfit after eating.
Chinese herbs and our Geelong acupuncture treatments can relieve a wide range of digestion problems and discomfort, including:
To try and prevent digestive issues in the first place, it’s important to choose a healthy diet. A healthy diet changes depending on each person, and also incorporates lifestyle decisions. Our Chinese medical practitioners can recommend tips to improve gut health and boost digestion, including:
In Chinese medicine, there are two factors for sickness:
Symptoms of sickness are a result of the body fighting against the external pathogens. If the body is healthy and strong, a person might experience mild symptoms or not get sick at all. However, if the body is not strong enough or the pathogen is vicious, symptoms can be very severe.
Allergic reactions are caused by the competitive onset of similar symptoms. They are allergen-induced, seasonal or not seasonal. In Chinese medicine, an allergy is a chronic condition that indicates the body is fighting against pathogen(s), but not strong enough to completely rid it from the body.
Allergens are found in a variety of sources. Common allergens include:
Allergic reactions can be triggered by any form of contact with the human body, including breathing and inhaling, consuming food or drinks and direct contact with any part of the body. Symptoms can include rashes, hives, nausea, vomiting, stomach pain, difficulty breathing, dizziness and some more serious conditions.
Hay fever refers to a complex of symptoms including sneezing, itchy eyes and nose, nasal congestion and runny nose in response to allergens such as pollen and dust.
In Chinese medicine, lungs are the primary organs for breathing. When lung Qi is insufficient, the lungs fail to expel external pathogens. That’s why a lot of people find their hay fever symptoms are worse when they also suffer from some other health problems, such as low energy and poor digestion.
There are two aspects involved in treating hay fever; reducing exposure to pathogens and minimising signs and symptoms. Keeping away from allergens is an effective way to prevent hay fever. Keeping windows and door closed during hay fever season, washing hands and face after going to the garden and tumble drying your clothes can reduce your exposure to pollens and dust.
We use acupuncture to reduce symptoms such as itchy eyes, nose and throat, blocked and runny nose and sneezing. We also give Chinese herbal medicines to moderate immunity and strengthen the lungs, to treat the root of the problem.
During non-hay fever season, it is necessary to strengthen the body’s defensive Qi, and improve constitution.
Acupuncture is covered by
Please note we charge a discounts fee to patients whose treatment is covered by Worksafe or TAC. You can claim part of the fee back from them.
Chinese herbal medicine consultation and herbs are covered by some private health insurance companies. Please check your cover schedule.
Your first appointment will be 60 minutes, including a 30-minute consultation and 30-minute treatment session (if you have acupuncture treatment). This will enable us to establish a solid history and have a good understanding of your condition.
Follow up appointment will be 30 minutes in most case and can be 45 minutes in other cases.
Once you make your first appointment, prior to your first visit, you may want to write down your health history, including surgeries, injuries, allergies and medications you are on. Please also write down how the current problem was developed and how it has been investigated and treated. Please bring the information to your first appointment.
We recommend you wear comfortable clothes that roll up to knees and elbows, or are easily removable.
Do not come for acupuncture treatments on an empty stomach / too full a stomach or having consumed drugs or alcohol.
Chinese medicine or acupuncture consultation inquires many aspects of your life, such as sleeping patterns, digestion, emotional state, diet, and lifestyle. Unique to Chinese medicine diagnosis, your tongue and pulse may be examined, and areas of concern may be palpated.
Once a Chinese medicine diagnosis is made, we will develop the treatment plan with you that is most suitable to your situation. The treatment could be acupuncture alone, herbal medicine alone or a combination of both.
Please feel free to raise any questions or concerns at any time.
The prognosis, and the amount and frequency of your treatment depend largely on the severity of your health condition and how long it has been a problem.
Generally 1-2 acupuncture treatment sessions per week for 3-4 weeks are required to achieve a satisfactory result for acute problems. For chronic problems, it often requires weekly or fortnightly treatment over some months for progressive results.
With Chinese herbal medicine, formulas to restore chronic conditions may require weeks or months of use, whereas formulas for acute colds, cough or digestive problem can show positive results within a few days.
While you may gain immediate benefits even after one treatment, progress in health conditions is usually measured over a course of treatments, which involves 4-10 treatment sessions. This is done to ensure:
Follow up appointment is often 30 minutes including a short consultation to check any arising issues and treatment.
Acupuncture at Geelong Chinese Medicine Clinic follows well-known and popular traditional Chinese techniques involving the insertion of fine needles into the meridians of patients’ bodies. One of our most popular treatment options, acupuncture complements the range of therapies and Chinese herbal medicine at our Geelong clinic.
Acupuncture has its origins in China about 100 BC and involves stimulating body walls such as skin and muscle to produce therapeutic effects. Acupuncture can help a wide range of conditions, ranging from acute and chronic pain through to respiratory, skin and gastric problems.
To help understand acupuncture, imagine your body is a living city comprising organic highways and byways. When your city’s roads and paths are clear and traffic unimpeded, everything flows smoothly and easily. However, if there is a breakdown on any of those thoroughfares, the traffic flow becomes compromised and a traffic jam eventuates. If the breakdown remains uncleared, the traffic jam becomes worse and its effect on the city – your body – increases.
In your body, the roads and pathways are known as meridians, and the traffic along those meridians is an energy flow known as chi. Suffer an injury and the consequential response of your body, such as a muscle spasming or tightening, can create a traffic jam and block the chi flow.
Acupuncture treatment at Geelong Chinese Medicine Clinic aims to restore the chi flow and diminish the effect of the injury or illness. Our practitioners insert acupuncture needles into the affected area to help clear the traffic jam but will also insert needles into other areas to divert traffic away from the jam and help restore the chi flow.
Acupuncture has been proven to be effective for a number of pain and non-pain conditions common in primary care, and acupuncture for pain treatment at our Geelong clinic regularly brings relief to clients. We treat patients with a wide variety of complaints such as:
Evidence supports acupuncture’s benefit for anxiety, depression, insomnia, ulcerative colitis and it provides the opportunity for non-drug therapies for a number of health conditions. Acupuncture at Geelong Chinese Medicine Clinic can be easily integrated into multidisciplinary management of chronic conditions.
Please watch the video of our clinic’s Geelong acupuncture practitioner and RMIT University academic Dr Zhen Zheng explains how acupuncture treatment works.
Well-trained and highly experienced practitioners provide acupuncture at Geelong Chinese Medicine Clinic and patients should experience minimal discomfort during treatment.
While traditional Chinese acupuncture is a popular and effective treatment, our clinic also offers laser and electrical acupuncture in Geelong for those who have a fear of needles.
Geelong Chinese Medicine Clinic practitioners are also qualified to provide point injection treatments in which saline can be injected into acupuncture points to enhance therapeutic effect. We also provide scalp acupuncture, hand and foot acupuncture, wrist and ankle acupuncture, and micro-system acupuncture.
We encourage you to contact us to make an inquiry about our acupuncture treatment or other Chinese therapies such as cupping and moxibustion, Qigong and Chinese herbal medicine at our Geelong clinic.
As well as offering traditional Chinese acupuncture at our Geelong clinic, our practitioners also provide a range of needle-free treatments, including electrical acupuncture and laser acupuncture. Needle-free acupuncture is a popular and effective choice of treatment for those who are afraid of needles and complements the range of traditional Chinese medicine at Geelong Chinese Medicine Clinic.
Also known as electro acupuncture, electrical acupuncture involves the use of weak electrical stimulation to enhance therapeutic effects. It has been proven to be particularly effective for painful conditions.
This is another form of needle-free acupuncture and involves the use of low-power laser beams on acupuncture points in the body. Laser acupuncture has proven effectiveness for a wide range of conditions.
This is your “take away” treatment. We tape ear seeds onto your ear. The seeds can be in place for up to one week. This will enhance and prolong the effect of acupuncture.
Whether it’s illness, disease, discomfort or pain, Chinese medicine in Geelong is our expertise. Please contact Geelong Chinese Medicine Clinic to find out more about our range of services and treatments or to book an appointment.
At Geelong Chinese Medicine Clinic, we offer various non-invasive treatments. Each treatment is based on a person’s unique symptoms and needs. We believe in taking a holistic approach to your health, combining the use of Chinese herbs and treatments to restore your body’s natural harmony and promote overall well-being.
Traditional Chinese medicine (TCM) focuses on your mind-body-spirit connection. All aspects must be synchronised and working in harmony for optimal health and body function. There are many different treatment options available to help restore various functions of the mind and body, including a range of non-invasive acupuncture and related therapies.
Commonly used to treat muscle pain and tension, gua sha is an alternative massage therapy that involves scraping skin to increase blood flow and boost circulation.
In traditional Chinese medicine, the uninterrupted flow of Qi through the body is vital for health and wellness. Gua sha addresses stagnant Qi to reduce inflammation and promote healing.
Based on principles dating back more than 5000 years, the Chinese herbal medicine at Geelong Chinese Medicine Clinic has stood the test of time. As much about illness prevention as it is treatment – Chinese medicine involves practitioners taking a personalised approach to the prescription, preparation and dispensing of medicines specifically tailored to individuals and their health.
Chinese medicine adopts the premise that no two people have the same physiology and therefore will not display precisely the same symptoms for illnesses and diseases. Consequently each individual might require a different prescription of Chinese medicine even though they might have the same health condition as others.
The clinicians at Geelong Chinese Medicine Clinic will prepare and recommend Chinese herbal medicines suited to each person’s unique needs, including
Chinese herbal medicine refers to plants, animals and minerals grown in the natural world or processed from natural products. The majority of medicines are plants, which is why we generally call them herbal medicine. In the long history of Chinese medicine practise, there are over 3000 individual herbs listed in the Chinese Medicine literatures, and about 200 to 300 of them are commonly used in today’s practise.
Chinese herbal medicine is applied based on Chinese medicine theory – including Yin and Yang theory, five element theory, Qi, Blood and water metabolism theory – to strengthen weaknesses and purge excesses, warm the Yang and reinforce the Yin to balance out the body.
Herbs grow in different environments and each has a different taste and property. In Chinese medicine, herbs are used according to taste and property.
For example, ginseng grows in a cool environment and has a sweet taste. It is used to warm up the body and reinforce the weakness for people recovering from bad injuries and diseases. Dandelion, a very common weed growing in our backyard, has a bitter taste and it grows very well in warm seasons. Dandelion is cooling and purging, used in treating infection, inflammation and abscess and detoxifying the liver and stomach.
In practise, a formula (a group of herbs) is usually given instead of an individual herb on its own to maximise the treatment effect.
Chinese medicine is an individualised medicine. People with different diseases can be given the same herbs, while different herbs can be prescribed to treat the same health issue in different people.
Chinese herbal medicine can help improve a wide range of health problems, from sleep problems to digestive issues, stress and hay fever and other allergies. At Geelong Chinese Medicine Clinic, we believe in using Chinese herbal medicine to relieve sufferings as well as improve overall health and well-being in order to prevent the imbalances in the body that lead to disease and other health concerns.
A peaceful mind, body and spirit is the binding principle of Chinese medicine. If there is even a small imbalance in any part of the body, it can disrupt the flow of energy, resulting in pain or sickness.
The Chinese medicine practice focuses on patterns of signs and symptoms and the mechanisms behind these symptoms – which is the dynamic balance of Yin and Yang, Blood and Qi movement as well as the visceral organs.
Using a combination of Chinese herbal medicine and acupuncture, our practitioners help restore your body to optimum function, as well as reduce pain and other symptoms of disease, sickness and other health concerns.
At Geelong Chinese Medicine Clinic, a Chinese medicine consultation generally takes about half an hour. We need to know about your very detailed health history as well as your general health conditions. We also read your tongue and pulse to get a whole picture of your body and then make an individualised formula to rebalance it. We have both powder herbs and patent herbal pills to suit the individual need.
Cupping is a long-practised treatment used in traditional Chinese medicine (TCM). Cupping involves placing vacuum cups on the skin to create suction. This pressure is used to stretch skin, tissue and tight muscles upward. The suction assists healing by relieving muscle tension, increasing blood circulation, and with it the flow of “qi” in the body (Qi is a Chinese word meaning life force).
Cupping is often practised alongside acupuncture but can also be used as a treatment in its own right.
Cupping is not painful, however it can leave temporary reddish-purple patches on the skin that look like bruises, especially if there is an injury or energetic blockage under the area that was cupped. The discoloration on the skin shows there has been movement or change in the circulation of blood in the treated areas. Although these marks resemble bruises, the muscles are not injured. The skin discoloration can last from a few days to a couple of weeks, but is rarely painful.
Traditionally, cups were made from animal horn or bamboo, and later on from ceramics. Modern cups for vacuum cupping include glass, plastic, rubber and silicon; all with various ways for removing the air inside the cups and creating a vacuum, such as fire, hand pump, balloon or compression. There are two main methods of dry cupping (which is a suction-only method) used at Geelong Chinese Medicine Clinic:
Cupping has long been used to treat a wide variety of conditions. While cupping can be especially effective at easing muscle aches and pains, the cups can also be applied to major acupressure points, influencing the treatment of conditions commonly treated with acupuncture. A 2012 review of cupping therapy found that cupping therapy may help with a variety of conditions, but acknowledged more high-quality studies were needed to assess the true effectiveness of cupping.
A review of cupping therapy clinical trials showed cupping may help in certain conditions under the following areas:
While considered relatively safe if applied by appropriately qualified practitioners, cupping is a specialist technique and is contraindicated in certain cases. It is therefore very important to visit AHPRA-registered practitioners. All practitioners at Geelong Chinese Medicine Clinic are registered with AHPRA and are highly experienced in applying cupping. Based on your condition and preference, we will choose the best cupping method for you.
Moxibustion is a form of heat therapy, as Chinese medicine understands some presentations are cold in nature, whereas others are hot. Moxibustion uses a heat generating herb to produce warmth. There are a number of forms of this therapy.
This is the modern form of moxibustion to produce warmth. This therapy is effective for any presentations that Chinese medicine considers with a cold nature. This is different from commonly used heat packs.
Traditional Chinese Medicine (TCM) is based on the view that the body is interconnected. Due to this interconnectedness, all symptoms are related. For example, muscle tension could be related to diet, sleep, stress, emotion or other factors. It is an imbalance of these lifestyle factors that is the cause of all health complaints. Therefore it is the regular everyday things that most help maintain this ‘balance’ (Yin, Yang) or health of the body. These lifestyle areas can easily be understood as the way the human body ‘recharges’, but Chinese medicine principles about this idea can seem slightly different to what we’re used to.
These basics of a healthy lifestyle are:
While we are bombarded with many different and often-changing points of view about a healthy diet, food affects our health much more than the medicine we take. In Chinese medicine, diet is a key factor in maintaining health or recovering from illness.
Chinese medicine classifies food according to its energetic effects (such as warming and nourishing / cooling and eliminating) rather than just its nutritional parts. Patients are always advised to eat seasonal, unprocessed foods where possible and include multiple colours and flavours of a variety of healthy foods according to their individual constitution, ability to digest, and need for building certain deficiencies or decreasing an unwanted excess of “sometimes foods” (highly processed/ high sugar/ fats or toxic e.g. alcohol).
Due to this some foods may be seen as beneficial for some patients but unfavourable for others.
Moderate exercise (not too much and not too little) is an important factor, as physical activities are beneficial to the flow of Qi (energy) and blood, helping to maintain the body. Yoga, Tai Chi and Qi Gong are commonly recommended along with other exercises like swimming, walking, jogging and going to the gym.
TCM advises different types of exercise based on the individual patient’s constitution. Sometimes certain exercises should be avoided if too strenuous for recently ill or injured patients, and replaced with more suitable exercises like walking or Qi Gong.
Another essential, easy-to-understand principle is getting regular adequate sleep. Being sleep-deprived or having disturbed sleep patterns – whether actual sleep difficulties, shift work, or constant self-inflicted late nights – can weaken the body’s self-maintenance abilities, impact everyday function and can eventually cause illness.
Proper rest restores the body and mind, helping to maintain health and strengthen the body’s ability to resist disease. A balance between work, exercise, play and rest is something everyone needs. TCM principles also encourage stress reduction with relaxation through hobbies; appropriate socialising, exercise, and quality self-time help maintain balance.
Finally, TCM recommends conserving energy through understanding seasonal influences on body rhythms by modifying levels of activity appropriately (e.g. being more active in warmer months, but less active and more protective against exposure to weather in winter).
While TCM places a high value on diet and nutrition, it is also important to note “You are what you think.”
In TCM, specific emotions relate to specific organ systems. Negative emotions can directly impact the way an organ functions (especially digestion). Emotions like fear, anger, constant worry and overthinking are particularly disruptive if you experience them constantly. This is like a junk food diet for the mind. These affect your body’s ability to maintain balance. Mental stress-reduction through harmonious body, mind, and spirit activities like yoga, Qi Gong, meditation, and deep breathing exercises have long been used to help maintain a positive mindset.
Remember, in TCM, prevention is key. Making appropriate lifestyle choices means making good choices every day that enhance health and help prevent disease. Many health factors are in our individual control, through quality food choices, moderate exercise, restorative sleep, positive mindset, minimising toxins and stress management.
Research demonstrates that many chronic diseases are largely caused by lifestyle choices and habits. The important principle of preventive health care is that one can use lifestyle to bring about balance and health.
For further reading:
Good Life Habits According to Chinese Medicine – Shen-Nong

A literal translation of the Chinese character Qi is air or breath. It is the energy that circulates within the body. Gong is the term used for any study or training which requires a lot of energy and time, work or self-discipline, or arts. Thus Qigong is arts of Qi, and a method to build up Qi.
It is known that the beginnings of the Chinese art of Qigong have a history that goes back thousands of years, though only a few historical documents remain today.
Qigong practices are designed to guide and induce the free flow of energy/ Qi throughout the body via integrated physical movement, mental cultivation and regulated breathing. These exercises once learnt can also bring about increased muscular efficiency, balance and coordination, improved breathing and blood flow, greater flexibility, a calm mind and improved immune system.
In China for many hundreds of years, many different practices of Qigong have arisen but they all come from the same fundamental theories based on the observation of nature.
In traditional Chinese medicine the flow of energy Qi along channels or meridians in the body is viewed as central to a person’s health and wellbeing, with illness being attributed to restricted or blocked Qi flow within the body. This concept provides the basis for acupuncture and Qigong.
Qigong emphasizes the cultivation of health through the removal of blockages in the mind and body. As observed by the ancient Chinese, running water never turns stale and a door hinge never gets worm eaten.
Paul teaches Qigong through Geelong City Yoga with Geelong psychologist Helen Handsjuk on Wednesday AM and through Geelong West Neighbourhood House on Thursday evening.
Qigong is a training system that helps to generate a smooth flow of Qi (internal energy) inside the body and then circulate it through the entire body. Qigong practices may differ through their focuses, medical/health promotion, martial or even spiritual.
During the Song dynasty (960-1279 A.D.), a Daoist named Chang San-Feng is believed to have created a martial art Taijiquan (Tai Chi Chuan), which means ‘grand ultimate fist’. Tai Chi shares Qigong internal Qi/energy principles because it emphasizes on working with qi.
When practiced slowly, Tai Chi is a form of Qigong (energy work) with Qigong health benefits, but Tai Chi is also a martial art. In every movement of Tai Chi, you can find a martial arts application that can be used for self-defence. Some forms of Qigong do promote physical characteristics useful for martial arts, but in comparison, Qigong lacks the attack and defence principles contained in the Tai Chi postures. So, to sum up, Qigong & Tai Chi work off the same principles. Tai Chi just expresses the ability to cultivate, circulate and harmonize Qi in relation to martial arts.
While, there are over 500 research studies on qigong, and over 1800 studies on tai chi, there are many challenges and complexities in studying and proving benefits of such practices, but the evidence for the health benefits of Qigong and Tai Chi is encouraging.
Here are some of the benefits of Tai Chi and Qigong as indicated through clinical trial evidence.
A video demonstration of the Qigong movements by Master Liu De Ming,
What is Cosmetic acupuncture?
Cosmetic Acupuncture uses acupuncture points and techniques to address skin structural changes (acnes, fine lines and wrinkles) and internal factors that are related to those changes. It combines the Traditional Chinese Medicine (TCM) principles with scientific understanding of the skin. In TCM, it is believed that facial complexion and the skin ageing process are reflections of the internal disharmony, such as digestive intolerances, hormone changes and / or oxidative stress.
Facial acupuncture has a long history in TCM, and acupuncture points used for skin enhancement were first recorded in Zhen Jiu Jia Yi Jing (256-82 AD). It is widely held that the Chinese empresses used acupuncture for facial rejuvenation and anti-ageing since Song Dynasty (960-1279 AD) according to the published book Facial Enhancement Acupuncture: Clinical Use and Application, written by Adkins (2013).
In the modern days, cosmetic acupuncture has gained its popularity as a non-invasive anti-ageing alternative globally. It is known for its facial rejuvenation effects. Clinical studies have shown that cosmetic acupuncture treatments can improve facial elasticity (1), enhance the skin appearance and moisture level (2), soften the acne scarring, fine lines and wrinkles. They can also improve skin local skin microcirculation (3) and reduce Melasma areas (brown patches) (4).
During a cosmetic acupuncture treatment, a holistic skin care is offered. Individualised plans are provided according to Chinese medicine syndrome differentiation diagnosis. Acupuncturist will complete the regular full-body acupuncture first to address the imbalance in the body and ensure free flow of Qi (energy), then move to the facial part of the treatment.
Other mechanisms of cosmetic acupuncture can be explained as the following:
After high-quality and ultra-fine acupuncture needles (range from 40-70 needles) are inserted into the facial areas of concern, microtraumas occurs. The body then senses these micro-wounds, which trigger a localised micro-wound healing process, including (1-4)
In general, small percentage (1-2.9%) of patients who received acupuncture treatments reported a few mild adverse effects in a multicentre survey, including small bleeding, haematoma (bruising), dizziness, fatigue and local allergic reaction (rare)(6)
Rarely there are side effects associated with cosmetic acupuncture. However, a short-term, superficial bruising may occur occasionally when dealing with sensitive skin or patient is taking blood thinners. Appropriate care and advice during and after the treatment can prevent or manage bruising.
Cosmetic acupuncture involves the client in an organic, gradual process, which is customised for each individual. It is not a substitute for a surgical ‘face lift’ or Botox injection. To achieve satisfactory effects, repeated weekly acupuncture sessions are required for 10-12 sessions.
Each cosmetic acupuncture treatment usually lasts much longer than a standard acupuncture treatment session as it will address both internal imbalance as well as the skin issue. At Geelong Chinese Medicine Clinic, each cosmetic acupuncture cession will take 90 min and offers of a holistic skin care, including

In general, small percentage (1-2.9%) of patients who received acupuncture treatments reported a few mild adverse effects in a multicentre survey, including small bleeding, haematoma (bruising), dizziness, fatigue and local allergic reaction (rare)(6)
Rarely there are side effects associated with cosmetic acupuncture. However, a short-term, superficial bruising may occur occasionally when dealing with sensitive skin or patient is taking blood thinners. Appropriate care and advice during and after the treatment can prevent or manage bruising.
Last weekend, I had the opportunity to attend an online conference from Hong Kong on Chinese medicine for COVID and long COVID. Tele-health delivery of Chinese medicine has been encouraged in Hong Kong during the pandemic. Chinese medicine practitioners from Hong Kong, mainland China United Kingdom of Britain, United States of America and other countries shared their experience of helping people with COVID and long COVID. Chinese herbal medicine is often used as it can be delivered with limited patient contact. Acupuncture was not possible, instead acupressure has been used. Patients are taught how to press on acupuncture points to achieve clinical effects. This form of self-care empowers people to gain some control over their symptoms and to build confidence and hope.
In this blog, we will talk about what acupressure is and how to use acupressure to help some symptoms associated with long COVID.
Acupuncture stimulates specific parts of the body, called acupuncture points or acupoints, with fine needles for therapeutic effects. Acupressure is a form of acupuncture, but without needles. It stimulates acupoints through mechanical pressure. The pressure can be delivered via human fingers, or some specifically made or home made pressure tools, such as chop sticks, pens, and tooth pecks. People can press acupoints themselves or let friends, family members or therapists to help. Acupressure is a highly useful self-care practice. It can be done
Acupressure helps alleviate some symptoms: such as headache, nausea, or feeling anxious; and promotes healing.
It is important to consult qualified Chinese medicine practitioners for which acupoints to press and how to stimulate those points.
According to a recent study from UK, the commonest long COVID symptoms are exhaustion or fatigue (73%), brain fog (63%), short of breath (55%), headache (47%), concentration (45%), muscle ache (45%), palpitation 40%, Dizziness (38%), and many other symptoms. Often people experience a range of symptoms.
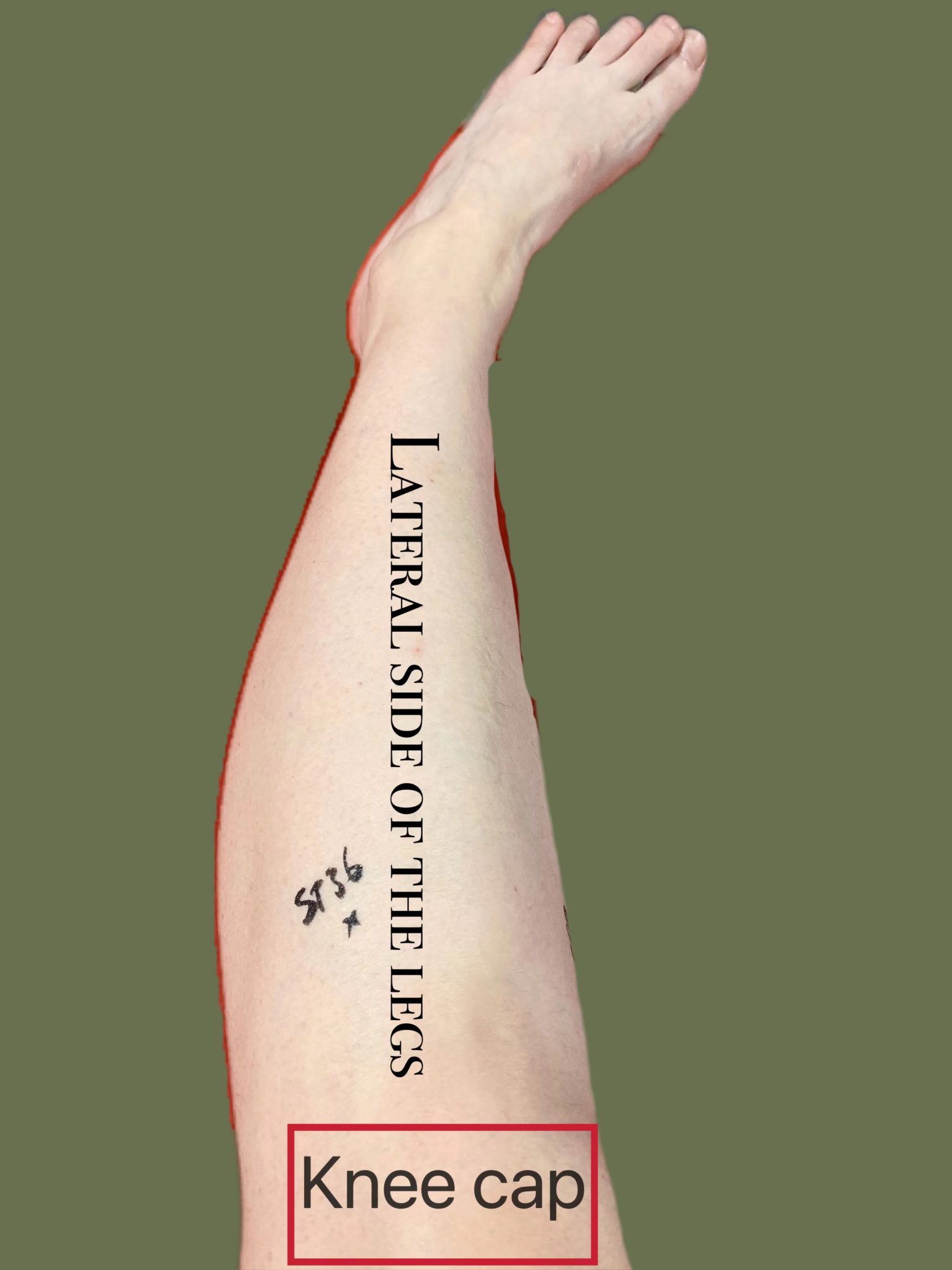
Below is a set of acupoints that can be used to alleviate various symptoms associated with long COVID. Photos of the location of those acupoints are at end of the table. Persistence is essential. Spend one to two minutes on each point, twice a day would be helpful. Again before using acupressure, it is important to consult your GP to exclude other possible causes of the symptoms.
| Symptoms | Acupoint | Location | Pressure , and Note | Notes |
| Headache / Blocked nose
|
LI4
SJ5 |
Between index and thumb
On the forearm, just above the wrist |
The pressure needs to be strong, to induce deep, diffused aching sensation on and around acupoint | LI4: Frontal Headache
SJ5: temple headache, In some people, headache could reduce relatively fast. For better results, one needs to attend to sleep, reduce or stops using caffeine, engage in gentle exercise. If your work involves lots of screen time, then take frequent breaks from the desk, and go to the nature.
|
| Fatigue | LI10,
ST36 CV6 |
LI10 on forearm,
ST36 on the legs CV6 just below umbilicus |
The pressure on ST 36 needs to be strong, to induce deep, diffused aching sensation on and around acupoint
CV 6 needs to be gently massaged or simply put palm on the acupoint to warm up the area and to draw attention to the area |
Fatigue is the very difficult to treat, and many factors contribute to it, such as sleep, use of caffeine, screen time, mental status, physical activity (too much or too little), and pacing.
Can add gentle massage on both sides of the legs and arms. Suggest continuing with acupressure and massage for long-term gain. |
| Muscle ache | LI4,
ST36, SP9 |
As above
On legs |
The pressure on the three acupoints need to be strong.
|
If you have sensitivity to pressure, then reduce the pressure or simply gently stroke the arms and legs. |
| Short of breath
|
Painful, or tight spots on the spine and both side of skin on the midback | Mid back | Stand against a wall and use a tennis ball to press on those points by rolling the ball up and down against the wall. 1 to 2 minutes. Twice a day
Put a warm pack on the back once a day for 10 minutes
|
Some forms of short of breath could be addressed by loosening up the muscles in the upper back area. Some stretching will be helpful. It is also helpful to have some spinal work with registered chiropractors, physiotherapists, osteopath or your trusted body therapists. |
| Foggy brain | Neck | The part of the neck just below the scull. | There are many acupoints in this region . However symptoms can get worse if not careful. So avoid acupressure there. Warming the area with your warm palm or wheat bag to the area; and keep this area warm with a scarf most time during the day.
|
In addition to long COVID, foggy brain could be related to sleep duration and quality; position of head; clearance of nasal passage; and breathing pattern; and / or dietary habit. All of these need to be assessed by qualified healthcare providers before more personalised approaches can be developed. Please also see previous blogs on Acupuncture for long COVID. |

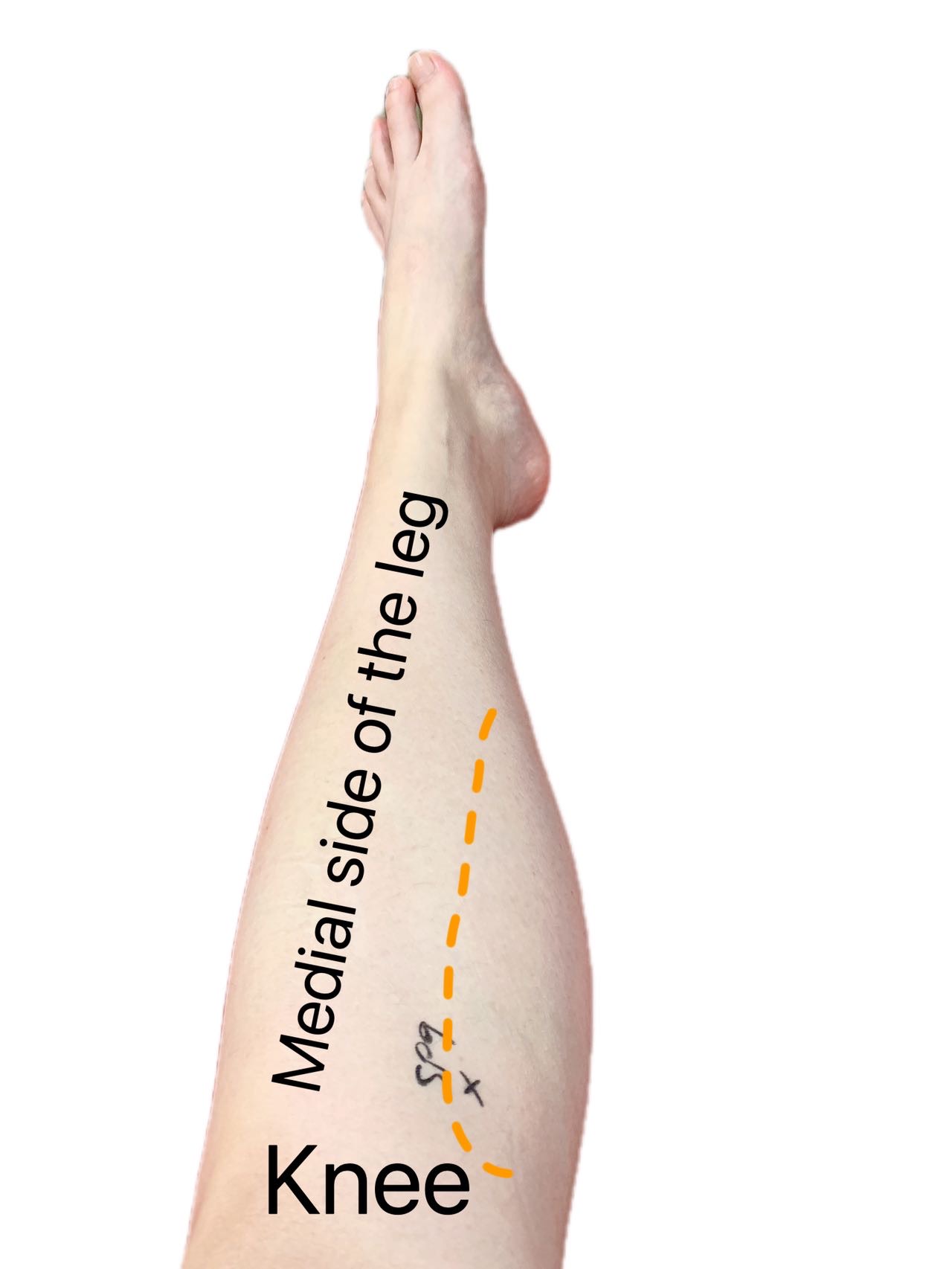
SP9 (Yin Ling Quan)
Since January 2022, in our Geelong clinic we have seen more and more patients who have had COVID-19. Some patients came to us within a few weeks of diagnosis, presenting with fatigue, brain fog, loss of smell, feeling cold and / or short of breath. Let us call this post-COVID condition. Others came to us weeks or months after the diagnosis, which fits in with in the diagnosis of long COVID. In the last blog, we talked about long COVID and its diagnosis. In this blog we will explain ours and others’ experience of treating post-COVID condition and long COVID with acupuncture.
How does Chinese medicine understand long-COVID?
Chinese medicine diagnoses health conditions based on detailed analysis of individual’s symptoms, with minimal reliance on laboratory tests. Using data from those who contracted the initial variance of SAR-CoV-2 virus (COVID-19 virus), Chinese medicine practitioners in China identified 10 common types of patterns based on different signs and symptoms presented. Even with the same variance of the virus, there are different patterns of presentations. This is because of individual differences in our constitution and body system, and in geographic locations.
Similarly, there are a few different patterns associated with long COVID based on our experience. The most common one is called Cold dampness, which suppresses the Yang or fire of our body. Our vitality, mental alertness and strength is the result of a balanced Yin and Yang. When the Yang is suppressed, Yin will be dominate, leading to a state of fatigue and inactivity. The presentation of cold dampness associated with long COVID is feeling cold easily, in particular in the upper body, tightness in the neck and / or chest, fatigue, heaviness in the body, feeling like having to drag oneself every day, mental fog, feeling fullness in the head or headache, body aching and tightness, either waking up un-refreshed or unsettled sleep. Some people also experience short of breath, cough or heart palpitation. Some people may have blocked nose or sinuses, loss of change of smell and taste, diarrhoea and / or abdominal bloating. Anxiety and depression, either new onset after COVID-19 or exacerbation of previous mental health issues, are very common. Chinese medicine sees emotional and physical health as one. So the combination of those symptoms is labelled as Cold dampness. This diagnosis helps Chinese medicine practitioners develop appropriate treatment strategies.
Some people might have fatigue, mental fog, but feeling hot. Then this will be a different pattern, with different treatment strategies.
How does acupuncture help long-COVID?

Acupuncture is used to strengthen the body, move the dampness out and unblock the meridians, or energy pathways. It is also used to calm the system, improve sleep and reduce pain. Moxibustion, a modality of acupuncture involving using a medicinal herb (Artemisia) to warm certain body parts, is used to expel the coldness and to activate Yang Qi. Together the two modalities are to rekindle the fire in the body and restore the meridian flow, consequently to address a number of symptoms associated with long COVID. So far two case reports have been published, and three clinical trials, one in the United Kingdom, one in the United States of America and one in Germany, are recruiting participants.
From modern science point of view, how might acupuncture help long COVID? To answer this question, we need to look at the current understanding of the pathology underlying long COVID. The knowledge in the field is developing as we speak. A 2021 paper published in the leading medical journal BMJ explains that inflammation status alone could not explain the presence of fatigue. The authors think that fatigue is likely to be the results of multiple factors involving the central nervous system, peripheral muscles, and psychology. Inflammation induced by SAR-CoV-2 virus could produce neural toxin and neuro-inflammation in the brain, direct viral infection of the skeleton muscles can cause damage to and weakness of the muscle fibres, and anxiety / depression itself often leads to fatigue. The review also points it that short of breath in some could be due to lung scarring after COVID-19, but many people with short of breath do not have evidence of lung damage. Another review states that short of breath, post-exercise fatigue, palpitation, chest pain and exercise intolerance could be due to autonomic nervous system changes or injury and persistent inflammation in the lungs. Un-refreshed sleep and sleep disturbance are so commonly seen among those with COVID and long COVID, the term “Coronasomnia” is proposed. Poor sleep quality could also contribute to the brain fog and fatigue. Overall multiple systems and mechanisms are involved in long COVID.
A recent systematic review outlines ample evidence supporting that acupuncture reduces neuro-inflammation, facilitates repairment of the nervous system, reduces pain and regulates the functions of multiple systems. A group of scientists from the Harvard University published a paper in the top science journal Nature in 2021 and discovered the specific mechanisms through which acupuncture reduces inflammation. Our recent systematic review in one of the top sleep journals has also shown that acupuncture changes the objective sleep index and has the potential to restore the sleep architecture among those with primary insomnia. It is important to know none of the research is specific to COVID or long COVID. However those proven mechanisms of acupuncture action provide some evidence base to our clinical practice.
How do we help people with long COVID?
For us it essential to work with your GP to help you with various symptoms associated with long COVID. It is important to exclude major health issues associated or not associated with COVID-19, such as pulmonary scarring, myocarditis, and cardia arrhythmia. A collaborative approach is likely to bring out the best result.
We will make a Chinese medicine assessment of individuals with long COVID. It is our opinion that fatigue and mental fog are closely related to the coldness in the body, anxiety, poor sleep or un-refreshed sleep, short of breath and blocked nose and head. We utilise the strengths of acupuncture and moxibustion to reduce anxiety, improve sleep, reduce pain, warm the body, and address other symptoms.
We have found for those who came to us early, soon after they were out of isolation, acupuncture can help alleviate symptoms faster and more effectively. For those who have developed long COVID for months, acupuncture help with alleviation of symptoms and improve functions at a slower pace. For those who have chronic fatigue prior to COVID-19, the changes are even slower. So early intervention is the key.
For some, it will be a relatively long journey to recover from long COVID. We will work with your GP and guide you to some self-care approaches, such as sleep hygiene, diet advice, self-acupressure (to unblock meridians), pacing and Qi Gong (for breathing and relaxation), so as to empower you on this journey.
Next time we will talk about some self-care strategies for post-COVID conditions and long COVID.

Feeling exhausted, brain fog, waking up feeling as if having not slept, or not able to get a sound sleep, feeling heavy in the body, short of breath, pain in the body and / or diarrhoea? Feeling blue; feeling anxious? Normal daily chores becoming too difficulty to complete; work getting harder as your brain does not seem to be as clear. This is now more than two or three months after the initial infection of SARS-CoV-2. You wonder if and when you will feel normal again; and if you will ever feel normal again.
If the above mentioned scenario applies to you, then you are not alone. What you are experiencing is called “long COVID”, a term was invented by people who still suffer from symptoms of COVID-19 weeks or months down the track. It was mentioned as early as March 2020 as “COVID long-haulers”, borrowing a term used by truck-drivers who work long shifts regularly. The World Health Organization (WHO) formally accepted this new condition and labelled it as “post COVID-19 condition” in October 2021 after an international survey of patients, researchers and experts in the field.
One in 10 to one in three people infected with SAR-CoV-2 could develop long COVID. Currently over 9 million Australians have had this virus, and about one to three million could suffer from long COVID as we are speaking. The Greater Geelong has in total about 97,000 cases since the start of pandemic, that is to say one in three Geelong residents has had COVID, and one in 30 to one in 10 could suffer from long COVID in one way or another, presenting a significant challenge to individuals and to the healthcare system. This debilitating condition is more common in adults than in children, more common in people who were hospitalised for COVID or those who have pre-existing underlying chronic diseases. However every adult who has had COVID-19 could develop into long COVID even they had no symptoms or mild symptoms at the initial infection stage.
There is no definitively diagnostic tool for this new condition. To meet WHO’s definition of post COVID-19 condition, one must meet the following criteria
Those symptoms may fluctuate or relapse over time.

It is essential that individuals check their symptoms with their GP to rule out organ damages or other health conditions. How long COVID is developed or for how many more months the symptoms might present is unknown at this stage. Consequently here is no effective treatment. At Geelong Chinese Medicine Clinic, we have been using acupuncture to treat the symptoms associated with long COVID with some good results. Our observation is consistent with the limited case reports in the literature on the use of acupuncture. So far no clinical trials have been conducted to examine the effect of acupuncture.
Our experience is that acupuncture is safe, and offers alleviation and hope to individuals. Symptoms like bodily pain, headache, diarrhoea, abdominal pain, and sleep disturbance respond well to acupuncture. We also see improvement in sleep disturbance and brain fog. It is pleasing to see that acupuncture could help people to gain some function back or to facilitate their recovery.
In the next blog, we provide our understanding of how acupuncture might be able to help long COVID; and what one could do to help themselves.
As the prevalence of common cold and flu increases in this winter, more and more people suffer from dry cough either during their illness or as a result of their cold or flu. Recently I was sick for over one week, from acute viral laryngitis. I rarely get sick. For someone who does not get sick easily, there is a lot to learn from being unwell. Although I dish out advice to my own patients, I, however, have to experience it to know how to walk the walk. Here I share my learning with you.
Having plenty of rest regardless how I feel. This is easily said than done. I did not have fever or bodily pain and I felt I could keep working. So I did. I was surprised that I did not really feel the tiredness even I did not have much sleep at night from dry course. On reflection, I wonder if my sense of being energetic had a lot to do with the urgency at work, and ginger tea or occasionally coffee I drank. All of these drinks would have energised me and masked how I felt. It might be a good idea to be off coffee or tea so as to give your body
the chance to rest.
Drinking warm water. We know keeping ourselves rehydrated being essential when we have a common cold or flu. But we must drink warm water as it is better than cold water for rehydrating and it sooths our dry, itchy or irritated throat. Hot water with fresh lemon juice
and honey is very soothing and help break down phlegm.
Avoiding spicy food or hot food if I have sore throat. I started with sore throat. It got a lot worse after I had a hot pot for dinner. The sore throat kept me awake at the night. Irritants to be off the list when one has sore throat are:
a. hot pot,
b. spicy food or food with chilli, and
c. fried food.
Accepting my health status and be patient. This was the hardest one. Being a Chinese medicine practitioner, I thought I knew how to look after myself and expected a speedy recovery. It was also very difficult to accept that I was sick at all. Chinese has a saying “Shao
An Wu Zao”, meaning “slowly calming down and having a peaceful mind”. This is the attitude I ought to adopt, and to accept I too could be sick, and I ought to let the virus running it course.
Exploring other factors could causing dry cough, and tickle in the throat: If you only feel itchy in the throat at night when you are in bed, then there could be other things tickling your inflamed throat.
a. Check your bedroom for dust, mould, dust mite or allergens. If you open the window during the day, it might be a good idea to use air filter to clean the air before going to bed. Pollens could easily get into the room when the window is open.
Other strategies for dry cough at night: Dry cough due to itchiness in the throat was the hardest part of my journey of being sick. I know the dry cough could last for weeks or months if I am not careful or do not address is as early as I can. Those night dry coughs are
very disrupting to our sleep, and our partner’s sleep. Those coughs are often hacking cough, dry, and took a while to settle down. Here are other strategies.
a. Sleeping in a half-sitting position if you also have nasal congestion. Tickle could come from nasal discharge running at the back of the throat. So the incline posture helps the nasal discharge to drain easily, reducing the amount of mucus congested in the throat, causing more irritation. Also when the throat is congested, we open our mouth to breath, which will further dry the throat, causing dryness or tickle.
b. Wear a thin scarf in bed as the nap is likely to be exposed to the cold air. Some people say I do not feel the cold. Well an inflamed throat will be super sensitive to temperature change, even 0.5 degree will make the difference.
c. Make the bed warm, before getting into bed. The lungs are between the chest and upper back. Keep those areas warm will keep the airway open more easily. You can put a hot wheat bag on the bed before going into bed.
d. Keep a flask of warm water next to your bed as the water will sooth the dry, tickly throat when you needed.
e. Sucking on lozenges is helpful as it will continue to rehydrate your throat; the lozenges having local anaesthetics could be more helpful.
f. Minimising talking and no singing throughout the day, in particular at night, to reduce the irritation.
Persistent dry cough is very draining. Hope those strategies will aid to your management. If your cough persists, you should seek advice from healthcare professionals. At GCMC, we often achieve good results from using acupuncture and Chinese herbal medicine for persistent dry cough residual from common cold, in addition to the above mentioned strategies.

Most pregnant women (half to two-thirds) will experience morning sickness in the first trimester. The degree of morning sickness varies from mild to severe (hyperemesis gravidarum). The symptoms include nausea, vomiting, loss of appetite and psychological effects (anxiety and depression) (Better Health Channel, 2022; Murkoff, 2016). Morning sickness is generally worse early in the day, but not limited to the morning. It can be anytime during the day or night (Better Health Channel, 2022; Murkoff, 2016). For most women, the morning sickness symptoms will reduce when entering the second trimester. However, few may suffer from them for the entire pregnancy (Murkoff, 2016).
The cause of morning sickness
The cause of morning sickness remained unknown. However, there are a few possible contributing factors (Better Health Channel, 2022; Murkoff, 2016):
How can we manage morning sickness?
Acupuncture or acupressure on the wrist
An acupuncture point called Nei Guan (PC6) is found helpful for nausea and vomiting (Ezzo, Streitberger & Schneider, 2006; Park et al., 2014). This point is located at three fingers above the wrist crease, in between the two tendons (Palmaris longus and Flexor carpi radialis) (Figure 1).
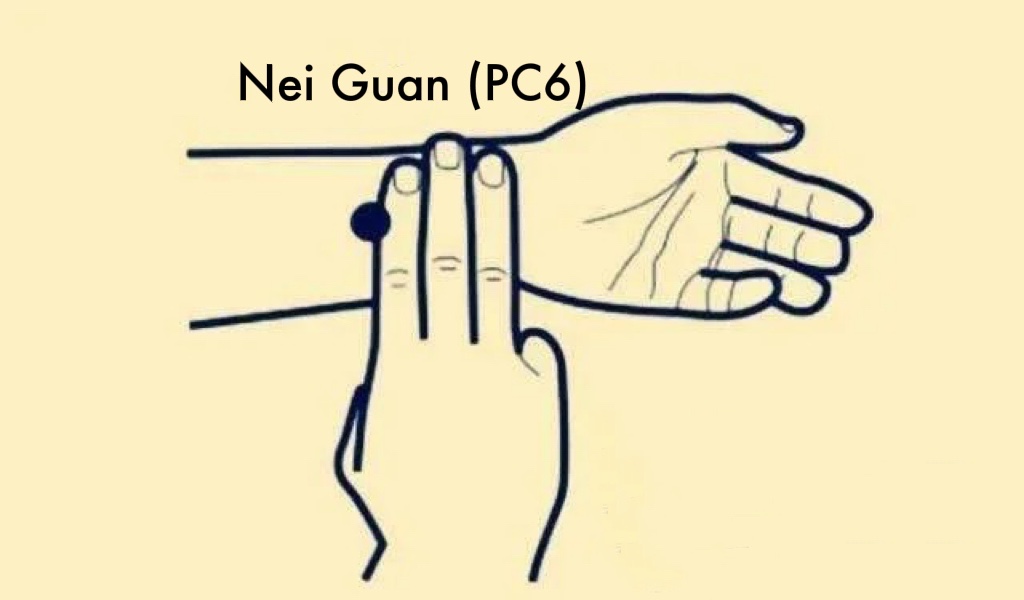
The Cochrane systematic reviews have reported that both acupuncture or acupressure on PC6 are safe to use during pregnancy when correctly applied (Ezzo, Streitberger & Schneider, 2006; Park et al., 2014). Acupuncture is one of the methods to stimulate PC6 for morning sickness. It is performed by licensed practitioners, who insert and manually rotate a very fine needle on the point (Ezzo, Streitberger & Schneider, 2006). Acupressure is another way for PC6 stimulation. It is a beneficial and safe self-care tool for morning sickness (Gürkan & Arslan, 2008).
How to perform acupressure?
Self-administration
Sea-band
Wear a Sea-bandTM (can be purchased from the local pharmacy) that an put pressure on PC6 has a strong effect on reducing nausea and vomiting (Ezzo, Streitberger & Schneider, 2006) (Figure 2). It can be removed at anytime if you feel uncomfortable (Ezzo, Streitberger & Schneider, 2006).

Based on Chinee medicine theory, there are different types of morning sickness. In Geelong Chinese medicine clinic, we use different methods to address the needs of the individuals, including applying acupuncture on PC6 and other acupuncture points that are important and safe to use during pregnancy to ease nausea and vomiting. We also educate our clients about acupressure and self-care to enhance the treatment effects on morning sickness. In the next blog, we will talk about acupuncture and pregnancy related anxiety.
References:
Better Health Channel. 2022, Pregnancy – morning sickness, accessed 14 June 2022,
< https://www.betterhealth.vic.gov.au/health/healthyliving/pregnancy-morning-sickness>
Ding, M., Leach, M., & Bradley, H. (2013). The effectiveness and safety of ginger for pregnancy-induced nausea and vomiting: a systematic review. Women and Birth, 26(1), e26-e30.
Ezzo, J., Streitberger, K., & Schneider, A. (2006). Cochrane systematic reviews examine P6 acupuncture-point stimulation for nausea and vomiting. Journal of Alternative & Complementary Medicine, 12(5), 489-495.
Gürkan, Ö. C., & Arslan, H. (2008). Effect of acupressure on nausea and vomiting during pregnancy. Complementary Therapies in Clinical Practice, 14(1), 46-52.
Murkoff, H. (2016). What to expect when you’re expecting (5th ed). New York: Workman Pub
Park, J., Sohn, Y., White, A. R., & Lee, H. (2014). The safety of acupuncture during pregnancy: a systematic review. Acupuncture in Medicine, 32(3), 257-266.
As the season changes, from summer to autumn, then autumn to winter, your body changes too. Some might feel tired, experience pain, have sleep disturbance or suffer from Seasonable Affective Disorder. From Chinese medicine point of view, the Yin and Yang balance is shifting during this transition, making our body in a vulnerable state to the temperature changes, shortened daylight, and virus or bacterial infection.
The Victorian Government recently announced the new rules of living in the COVID period. As of 22 April 2022, neither check in nor vaccine status is required when attending many venues. In addition, mask is no longer required in many settings except for a few. The mask rule has been there for over two years during the COVID-19 pandemic. This change is based on the high vaccination rate and low mortality of the new variant of COVID-19. It is a great milestone that we have achieved. We are on the pathway to regain our normal life. However we are far from out of the pandemic as COVID-19 virus continues to mutate and prevalent in the community internationally.
In addition, as we have been indoors in the last two years, our immune system could have been weakened. This winter many people will be more susceptible to flus virus and other common colds. Indeed at moment in Geelong, many people are sick, not from COVID-19, but from other common forms of virus.
So how do we protect ourselves this winter? One of the fundamental principles in Chinese medicine is “When the righteous Qi is within, evil Qi cannot invade our body”. The righteous Qi can be understood as the balanced or resilient immunity we have; whereas the evil Qi is those pathogens external to our body, such as virus or bacteria.
The key to strengthen our righteous Qi is to maintain a balanced Yin and Yang. In autumn and winter, there will be more Yin around us as the day is cold and the night is longer. The air could be dry, which often comprises the balanced state of our airway, making us vulnerable to virus that infect us through the airway.
Here are some tips based on Chinese medicine understanding on how to balance Yin and Yang during autumn and winter.
Apart from strengthening the righteous Qi, you also need to avoid evil Qi.
Ginger drink for winter
This drink is only suitable for people who feel cold in their body often and those catches cold easily. If you feel hot easily then do NOT use this recipe.
Put two cups of water in a pot, and add in the ginger pieces. Heat the pot it up until boiling, keep boiling for 3 minutes. Then turn off the heat. This process will reduce the water into one cup. Strain the water into a cup, sip the water when it cools down. You can sip the ginger water after breakfast and before lunch. I do not recommend sip the drink on empty stomach.
You may want to do that once every second day throughout the winter.
Autumn is upon us. The beautiful golden leaves of elms, orange displays of maples, red flushes of oaks … paint a beautiful picture of the autumn landscape. Almost everyone loves the beauty of autumn and the freshness in the air.

Do you know that the colour changes in plants signify a transition to the coming winter? In plants, there are many changes occurring during this time. We, the human, as part of the nature, too experience changes. As the night temperature drops, the day gets shorter plus the finishing of summer daylight saving, there are more darkness and coolness around us.
In Chinese medicine there is an increase of Yin elements in the nature during this transition. Most people will feel tired, some have disturbed sleep, some may experience increased pain and a small percentage, less than one in 100, could experience depression, known as Seasonal Affective Disorder (SAD). The seasonal cycle has greater impact on people who are sensitive to changes and people who are middle age or above. At Geelong Chinese Medicine, we see an increasing number of people suffer from the above mentioned symptoms in the last a couple of months.
In Chinese medicine, this is a crucial time to help body transiting to the next phase through balancing Yin and Yang that is specific to the season of autumn. To overcome the increasing Yin in the nature, we need to increase Yang activities in our life, if we have not done so.

We hope this information helps.
Mother’s day is coming. We wish that every mother will have a lovely day with family, friends, community and / or yourself. A beautiful scarf adding to the autumn colours could be a perfect, thoughtful gift to a mum.
In the previous blog, we provided some pre-conception advice. Today, we would like to talk about postnatal care.
In China, the postnatal care that involves dietary rules for 30 days after childbirth is called “Zuo Yue Zi” (sitting the month). “Zuo Yue Zi” was first recorded in the medical texts during the period of West Han Dynasty (206 B.C. to 25 A. D.) (Chen, 2011).
It is believed in Chinese medicine that women have given lots of vital qi to the fetus during pregnancy, and became yin and yang imbalanced after giving birth. As a result, they are required to be nourished and rebalanced. This replenishment can be achieved from taking specific diet (Ho, Li &Su, 2011).
Base on Chinese medicine theory, the general dietary rules during “Zuo Yue Zi” is to avoid (Ho, Li &Su, 2011):
On the other hand, food that considered to be “warm” is encouraged as this type of food can nourish organs (Ho, Li &Su, 2011). Three main ingredients are commonly used, including dry ginger, sesame oil and rice wine, which are all considered warm in Chinese medicine (Chen, 2011).
In addition, assisting breastfeeding is a crucial part of postnatal care. Globally, breastfeeding is the preferred method to feed infant due to its neonatal and maternal benefits. However, approx. 50% of young mothers could face lactation difficulties as a result of delayed breastfeeding initiation, painful breasts, invaginated nipple or emotional distress (Pierdant, et al, 2022).
A case study from Pierdant et al. (2022) indicated that both the body and auricular acupuncture can improve the onset of lactation, prompt milk production as well as enhance the serum prolactin level. Also, Mills et al. (2006) reported the Chinese medicine herbs, including Huang Qi, Pu Gong Ying, Tong Cao, Lu Lu Tong are commonly used herbs for enhancing milk production by boosting the vital qi, yin, and blood or unblocking channels, invigorating blood .
In Geelong Chinese medicine clinic, we normally prescribe herbs according to each individual’s condition to help with milk production, lochia discharge and uterus recovery (Ho, Li &Su, 2011). Here we would like to share some of the confinement soup recipes (Chen, 2011):
Ingredients: 20g raw red-skin peanuts, 50g red beans, 8 Chinese jujube (dried red dates), 6g goji berry, 20g brown sugar

Ingredients: 2 Pig’s trotter, 80g soybean, 6 pieces dry ginger, 6g goji berry

References:
Chang, P. J., Tseng, Y. C., Chuang, C. H., Chen, Y. C., Hsieh, W. S., Hurng, B. S., … & Chen, P. C. (2010). Use of Sheng-Hua-Tang and health-related quality of life in postpartum women: a population-based cohort study in Taiwan. International journal of nursing studies, 47(1), 13-19.
Chen, S. S. (2011). Zuo Yue Zi Sitting the Month in Taiwan: Implications for Intergenerational Relations (Doctoral dissertation, Case Western Reserve University).
Ho, M., Li, T. C., & Su, S. Y. (2011). The association between traditional Chinese dietary and herbal therapies and uterine involution in postpartum women. Evidence-Based Complementary and Alternative Medicine, 2011.
Mills, E., Dugoua, J. J., Perri, D., & Koren, G. (2006). Herbal medicines in pregnancy and lactation: an evidence-based approach. London; New York: Taylor & Francis.
Pierdant, G., Westphal, K., Lange, A., & Usichenko, T. I. (2022). Stimulation of Lactation Using Acupuncture: A Case Study. Journal of Human Lactation, 08903344221078802.
In Geelong Chinese Medicine Clinic, many patients have consulted us about what kind of things they can do to get ready before pregnancy. In today’s blog, we would like to give some general advice.



Acupuncture and Chinese herbal medicine have been used for hundreds of years in China to enhance fertility in women and men. In recent years, many clinical trials have been conducted to support the clinical observation. In our Geelong Chinese medicine, we provide individualized care plans to our clients who need fertility support. In our next blog, we will talk about what leads to yin and yang, or qi and blood imbalance, as well as postnatal care.
References
Bitzer, J., & Mahmood, T. A. (Eds.). (2022). Handbook of Contraception and Sexual Reproductive Healthcare. Cambridge University Press.
Sollis, S. (2015). Vitamin D deficiency and infertility: A Systematic Review. Student Works.143. https://scholarsarchive.byu.edu/studentpub/143
Xia,GC. 2009. 夏桂成实用中医妇科学 (Xia Gui Cheng practical Chinese medicine Gynecology). 中国中医药出版社 (Chinese TCM publisher).
In part 1, we explained the complex factors contributing to menopausal related insomnia, hot flushes and mood changes. This part 2 explains how Chinese medicine understands the complex interaction, and how acupuncture might provide a promising approach to comorbid depression and insomnia in perimenopause. For detailed information, please read a recent review by researchers from the RMIT University.
Chinese medicine view
Chinese medicine understands that pre-natal Qi determines our growth, maturity, fertility and longevity. It supports all other body functions as showing in Diagram 1. When we reach 45 to 55 years old, we experience a sharp decline in pre-natal Qi, leading to a sharp withdrawal of support to other functions and causing imbalance among those systems. This explains why we suddenly develop various signs and symptoms, such as sleep problem, hot flushes, and mental changes, and why pre-existing injuries or pains become worse.
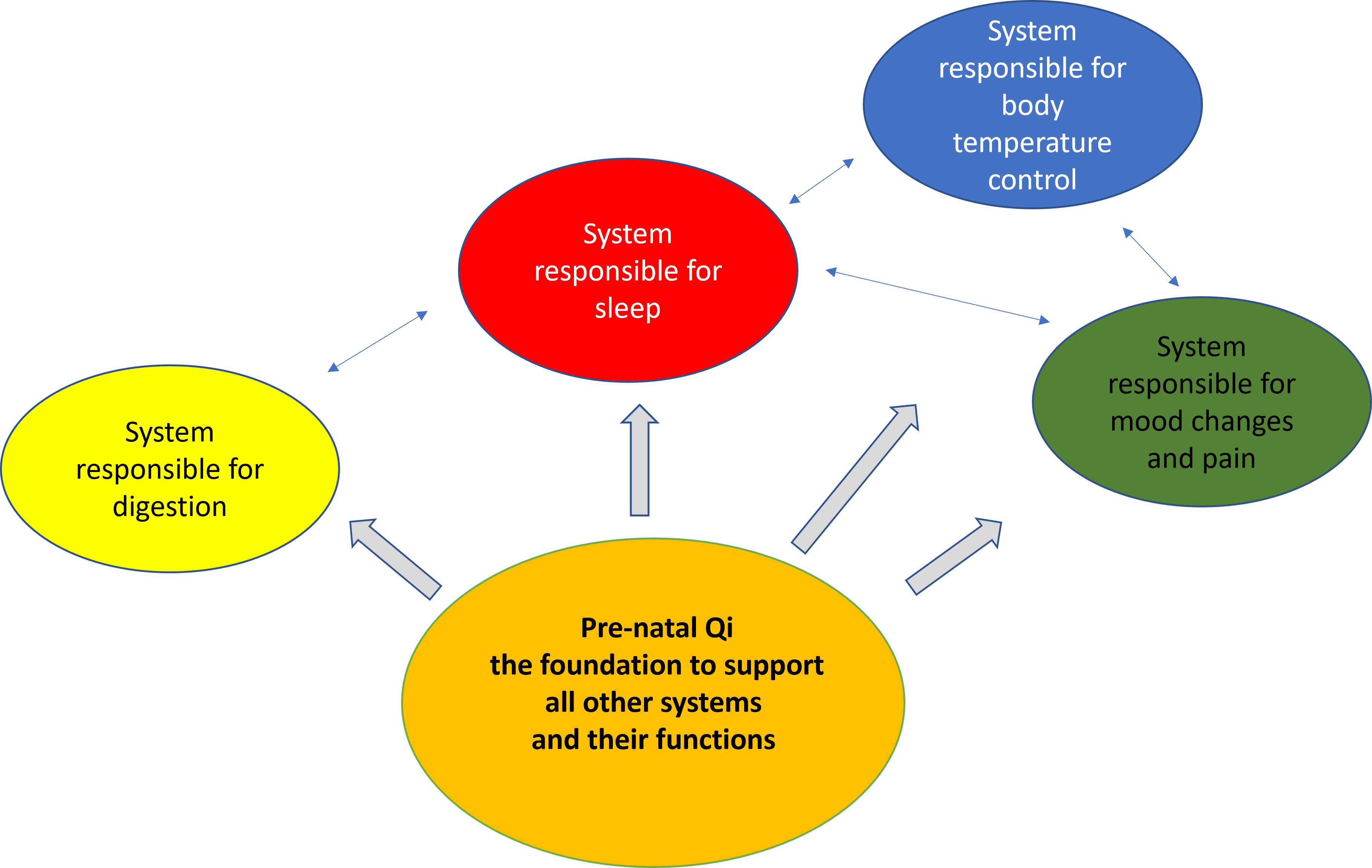
From Chinese medicine point of view, each person has a unique pattern of imbalance and varied combination of sleep, hot flushes, and mood changes. Some may have hot flushes and night sweats, feel irritable and anxious, and frequently waken up throughout the night; some may experience alternating hot and cold throughout the night, and stay awake after early hours of the morning, say 2-4 am; some do not experience any hot flushes, yet have difficulties in falling and maintaining asleep, feel depressed and experience lots of abdominal distension. Those different presentations are results of a combination of the pre-existing dynamic relationship among those systems prior to menopause and the current situation in our life, what we do, how we deal with issues in life etc.
In our Geelong Clinic, we develop individualised acupuncture treatment plans, and ways to address sleep hygiene. The effect of acupuncture can be explained by helping re-balance the dynamic relationship through
How does acupuncture work: Modern Science View
Modern research has found that acupuncture may improve perimenopausal depression and insomnia through multiple pathways: regulating reproductive hormones and their receptors; moderating neurotransmitters, signaling pathways, and oxidative stress; tone down hypothalamic-pituitary-adrenal and -ovarian hyperactivity. Of course, further research is required.
Evidence for effectiveness and safety of acupuncture
A significant amount of evidence supports the usefulness and safety of acupuncture. So far there have been over 30 systematic reviews and/or meta-analyses regarding acupuncture treatment for depression or insomnia. Acupuncture can be used alone or as an adjuvant therapy for patients with depression or insomnia, and could be particularly helpful to those who are intolerant to anti-depressants or hypnotic drugs. Acupuncture is safe when used alone or in combination with anti-depressants, and it may reduce the dose of medications. So far there is no acupuncture clinical trial that specifically addresses the combined depression and insomnia in peri-menopausal women. A RMIT multidisciplinary team is addressing this significant clinical problem.
What to expect
In all the clinical trials 8 to 16 sessions of acupuncture treatment with twice to three times a week treatment are required for a clinically significant effect. It usually takes 3-4 sessions to show some effects. Then the effect may continue to get better or plateaued. It is very important to be persistent in treatment for a sustained positive outcome.
You are a mid-age lady, approaching 50 years old. Life is suddenly turned upside down. You were energetic, had great memory and was switch on, then one day you suddenly find yourself being tired a lot, having poor memory, feeling not motivated or feeling anxious for no reason. The worst of it all is not able to fall asleep easily, wake up frequently throughout the night or wake up at 2 am or 3 am, then taking a long time to get back to sleep. You lie in the darkness, all thoughts trivial, unhappy, irrelevant or obsession run through your mind, keeping you awake.
If this describes you, then you are entering into menopause, and you are not alone. As mentioned in our previous blog, one in two perimenopause women experiences some forms of sleep disturbance, and one in three experiences depression or anxiety. The sleep problem gets worse after menopause (Baker et al 2018). Those who have surgical menopause due to removal of ovaries on both sides experience far worse sleep problems, reflecting the importance of a sudden change in female hormones on sleep quality. Linking to the changes in female reproductive hormone is hot flushes. Frequent hot flushes at night is closely related to perimenopausal insomnia.
Not all perimenopausal insomnia is, however, associated with hot flushes. Some insomnia is related to mood changes, such as depression or anxiety. The complex relationship among hot flushes, insomnia, and depression makes the treatment charllenging. For instance, anti-depressants used to treat depression can impact on sleep quality.
When considering peri-menopausal insomnia, one needs to consider the multiple factors, beyond those relate to hormonal changes. The diagram here describes an interdependent and interactional relationship among insomnia, hot flushes, and depression, and the many factors contributing to insomnia during perimenopause. Some factors (in blue) are related to menopause, whereas many are about women’s physical and mental health prior to menopause, lifestyles, and coping strategies. It is also important to note the significant impact from social factors during this midlife stage.
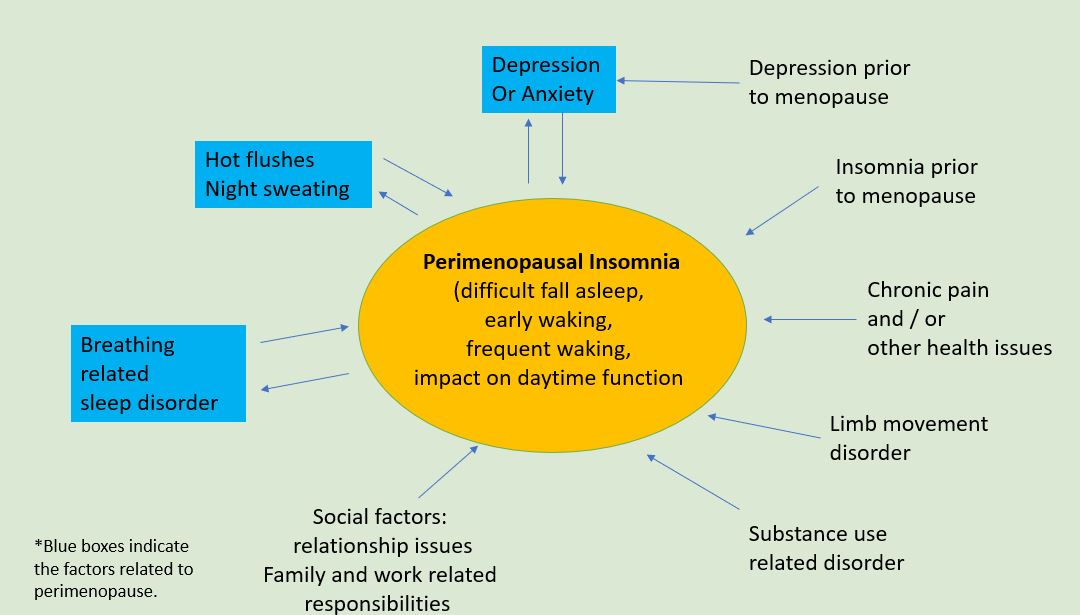
This diagram might also help you assess the specific factors related to your insomnia and how to address those non-menopausal factors. Perimenopause is the time for women to transit not only physically, but also mentally and socially. At Geelong Chinese Medicine Clinic, we encourage women to shift the transit to transform, and to not only turn the upside-down life back, but also to elevate the life to another level.
In part 2, we will talk about how Chinese medicine understands the complex interaction among hot flushes, insomnia and mood changes, and how acupuncture might provide a promising approach to comorbid depression and insomnia in perimenopause.

In the previous blog Fertility support in Chinese medicine, we talked about the importance of taking basal body temperature (BBT). Today I would like to briefly introduce the treatment principles used by practitioners in the Geelong Chinese medicine clinic to support fertility.
In Traditional Chinese medicine (TCM), regulating menstruation is very important in treating infertility as early, late or irregular periods can affect the ovulation timing (Liang, 2017). There are four phases of the menstrual cycle in TCM, and different treatment principles are given in each phase (Xia, 2009).
Phase 1: Menstrual bleeding period.
It is important to move blood circulation and resolve blood stasis in this phase. To make it easer to understand, we aim to “clean the house” so the earth is soft and fertile, in a condition that is ideal for planting (Liang, 2017; Xia, 2009).
Phase 2: Post menstruation.
It is the right time to boost blood and essence and prmopt mature follicles in this phase. Just like a farmer adding fertilizer to the soil so the seed can grow (Liang, 2017; Xia, 2009).
Phase 3: Ovulation time.
We focus on stimulating ovulation and dilating fallopian tubes in this phase. We are ‘unblocking’ the traffic so the trucks that carry seeds can get through smoothly when the soil is ready (Liang, 2017; Xia, 2009).
Phase 4: Post Ovulation (pre-menstruation).
We give acupunture or herbal treatments to strengthen the vital qi, warm the kidney and regulate the digestive systems in this phase. It is like the time when the farmers cultivate the crops, while still providing sufficient sun exposure and rain water (Liang, 2017; Xia, 2009).
It can be stressful and exciting at the same time when you are trying for a baby. If you need help, come to our Geelong Chinese medicine clinic for a consultation. We will make an individulised plan according to your own condition. Normally, we suggest 3 months (weekly visit) as one course treatment for fertility support .

References:
Xia,GC. 2009. 夏桂成实用中医妇科学 (Xia Gui Cheng practical Chinese medicine Gynecology). 中国中医药出版社 (Chinese TCM publisher).
Liang, D. 2017. How to Utilize Basal Body Temperature (BBT) when Treating Fertility According to Traditional Chinese Medicine (TCM). International Journal of Clinical Acupuncture, 26(1)
At Geelong Chinese Medicine Clinic, we encourage most of our patients to take up Qi Gong exercise for its broad benefits on mental and physical well-being. A 2021 news report from ABC narrates a few stories, ranging from how Qi Gong helps an Australian para-olympian back to racing to how it facilitates the recovery of COVID-19 patients in China. Qi Gong’s wide range benefits on anxiety (1), physical performance (2) and pain (3, 4) have also been supported by systematic reviews or clinical trials.
So what is Qi Gong? Qi Gong means the arts or the skills of Qi. It is a form a Chinese medicine exercise with slow, meditative moments. It regulates breathing and emotion as well as improving physical strength and reducing pain. Qi Gong could be understood as a foundation of Tai Chi, a well-known exercise in Australia.
People often think Qi Gong relaxes as most people feel calmer and relaxed after the practice. But is it really how Qi Gong works? A group of German and Chinese researchers set out to answer this question (5): Does Qi Gong relax or regulate? They examined the action of para-sympathetic nervous system (PSNS) and sympathetic nervous system (SNS) among experienced Qi Gong practitioners using the technology of heart rate variability. The researchers made three main findings:
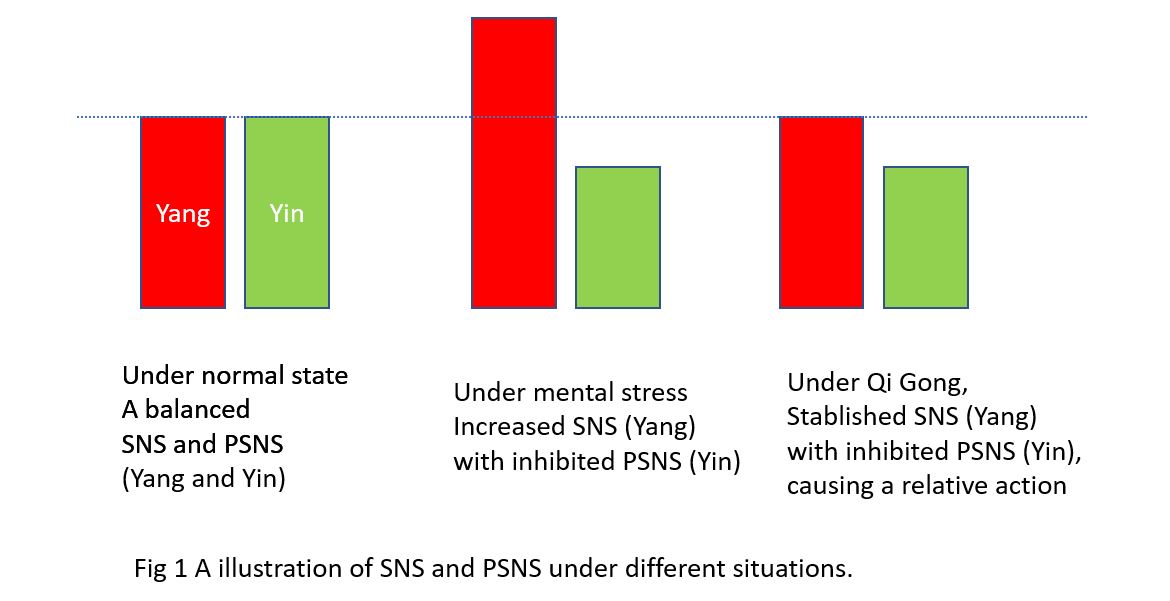
Let me interpret the findings with a plain language. The SNS is Yang as it is activated when we are excited and in action; The PSNS is Yin as it is activated when we are resting. A balance of Yin and Yang is the utmost harmonious state that people need to achieve.
Fig 1 illustrates the status of Yin and Yang under a normal, ideal situation, under mental stress and when practising Qi Gong. The findings show that Qi Gong induces the sense of vitality, not by enhancing the SNS (Yang) as that experienced under mental stress, but through inhibiting the PSNS (Yin). Practising Qi Gong leads to a combination of calmness and enhanced vitality, as if one is in a state of flow.
The researchers found that the alternating active and relaxing movements of Qi Gong is in synchronicity with the up and down regulation of the SNS and PSNS., i.e., there is a constant micro-regulation of the PSNS and SNS or Yin and Yang as shown in Fig 2, in which Yin and Yang is in a dynamic movement to achieve a balanced state as described in our previous blog.
To me this study is enlightening. Practising Qi Gong is like exercising your body’s capacity to regulate itself, to regulate the PSNS and SNS or Yin and Yang. Every time you do Qi Gong you are gently calibrating your Yin and Yang balance. What an amazing exercise!
References
What is infertility? WHO (2020) defines infertility as a disease of the male or female reproductive system by the failure to conceive after 12 months or more regular unprotected sexual intercourse.
Globally, infertility affects millions of people. Infertility can be caused by abnormalities of ovaries, uterus or fallopian tubes etc. for females, while by issues of semen ejection, low sperm count or abnormal movement and shape of the sperm for males (WHO, 2020).
Fertility support is crucial to prevent and assist the treatment of infertility. Yesterday I attended an amazing virtual international conference about the latest developments in Chinese medicine for infertility. Top Chinese medicine experts shared their clinical experiences with us. In today’s blog, I would like to talk about the importance of taking basal body temperature (BBT) based on Dr. DongYun Wang’s presentation.

Basal Body Temperature (BBT)
BBT is your temperature when you’re at complete rest. Your basal body temperature alters according to different factors, such as hormonal changes. (Su et al., 2017).
A few things need to be noted when taking BBT:
A BBT chart can tell your practitioner if you are ovulating, or if your temperature is too low or too high at different menstrual cycle phases, which guides your practitioner to choose appropriate treatments. Measuring BBT for at least 2 cycles is required.
A normal BBT looks like this (ovulation represents by a spike in body temperature) ( Xia, 2009)
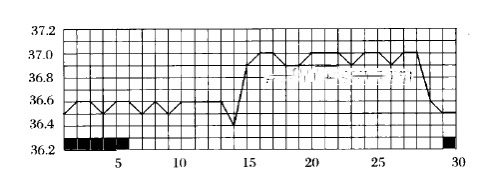
BBT is too low before ovulation ( Xia, 2009)
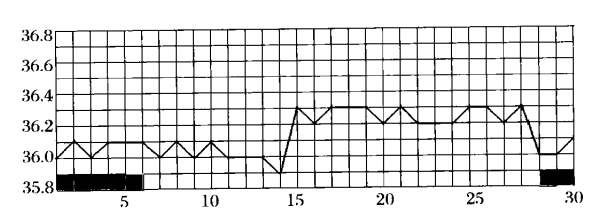
BBT is too high before ovulation ( Xia, 2009)
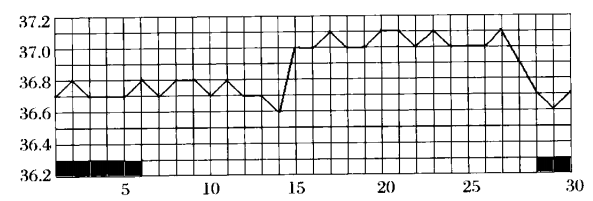
BBT is up and down before ovulation (stress-related) ( Xia, 2009)
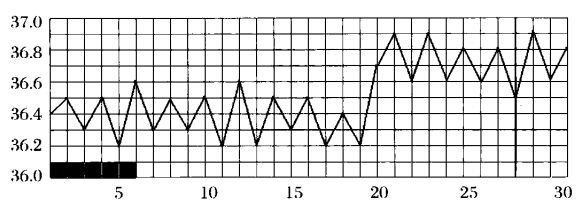
BBT helps to identify ovulation. However, the chances of getting pregnant are the highest 1-2 days before ovulation (Liang, 2017).
| Days before or after ovulation | Chance of conception (%) |
| 1 day before | 26 |
| 2 days before | 20 |
| 3 days before | 15 |
| 4 days before | 11 |
| 5 days before | 0 |
| Ovulation day | 15 |
| 2 days after | 9 |
| 3 days after | 5 |
| 4 days after | 0 |
Tracking cervical mucus changes is a good way to find out the days close to the actual ovulation. When you see egg-white like vaginal discharge , it indicates you are about to ovulate. This is the best time to conduct sexual intercourse.
In the next blog, we will talk about how Chinese medicine support fertility at different phases of the menstrual cycle.
At Geelong Chinese Medicine Clinic, our practitioners provide acupuncture or/and Chinese herbal medicine treatments to prepare your body, aiming to increase the chances of pregnancy. If you would like fertility support, feel free to consult with our practitioners.

References:
Xia,GC. 2009. 夏桂成实用中医妇科学 (Xia Gui Cheng practical Chinese medicine Gynecology). 中国中医药出版社 (Chinese TCM publisher).
Liang, D. 2017. How to Utilize Basal Body Temperature (BBT) when Treating Fertility According to Traditional Chinese Medicine (TCM). International Journal of Clinical Acupuncture, 26(1)
Su HW, Yi YC, Wei TY, Chang TC, Cheng CM. Detection of ovulation, a review of currently available methods. Bioeng Transl Med. 2017;2(3):238-246. doi:10.1002/btm2.10058
World Health Organization (WHO). Infertility. Retrieved from https://www.who.int/news-room/fact-sheets/detail/infertility
Do you know 97% of the Australian business are either operated by sole traders or by micro to small business owners, who experience more mental health issues than those working for large organisations or the average Australians. COVID-19 lock-downs have made this matter worse. Recent national surveys find that half to two thirds of small business owners are concerned about their mental health.
It is important to understand that mental health is NOT equal to lack of mental disorders. The World Health Organisation (WHO) defines that mental health is an integral part of Health, being a “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity”. This view is very similar to Chinese medicine understanding of how the unity of body and mind creates a balanced state.
Today I attended an excellent webinar delivered by Mel Novak from Beyond Blue on how to recognise mental health issues among small business owners, and what to do.
The top three reasons causing stress among this population are

Mel says it is important that we recognise what stresses us and check the signs of imbalanced mental well-being. Many mental health issues or their impact can be improved through preventive measures and support. Mental health is not a static state, it is on a continuum, varying from feeling the flow and flourish at work to feeling work being severely impacted. On this continuum, our mental state moves from one to another, and positive shifts can be made by simple strategies.
By tuning into signs, we can identify if our mind and body is stressed, impacting on our mental health, life and work.
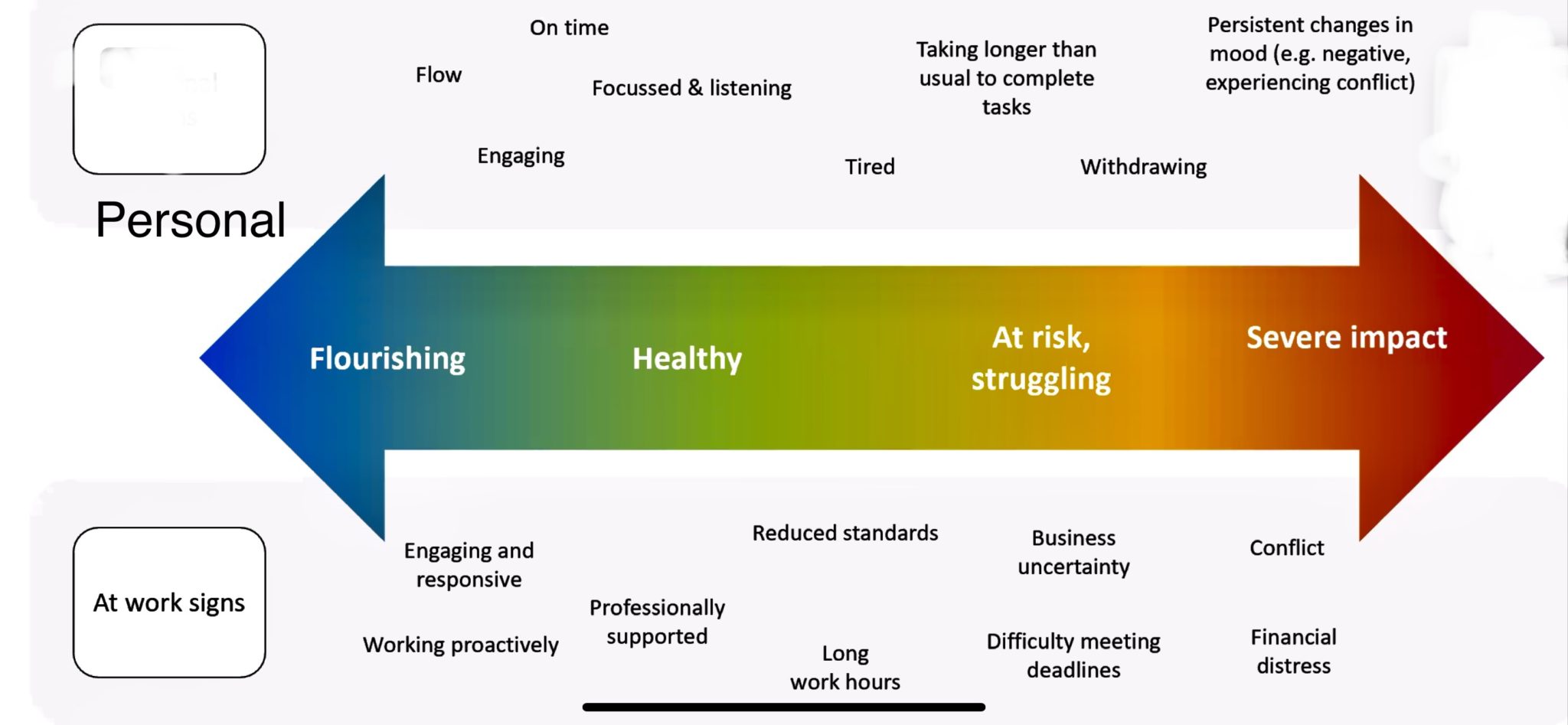
It is essential business owners looking after their own as well as their employees’ mental health status. Mel says that research shows for every dollar invested into mental health, the business gets $15 return through enhanced productivity, staff retention and high level of presence at work. Mel used bucket as an analogue for our mental health. If we consider our mind as a bucket, looking after our mental health is a bit like ensuring the bucket is filled with the right energy, prevented from being damaged, and gets repaired if it is damaged. Below is a summary of simple steps to how. As one can see, connecting with family and friends, ensuring physical health and the balanced mindset, avoiding negative information, seeking support, learning how to self-care and helping others are simple, yet very powerful strategies. Mel suggests that mental health is so important that a Well-being plan should be part of any business plan.
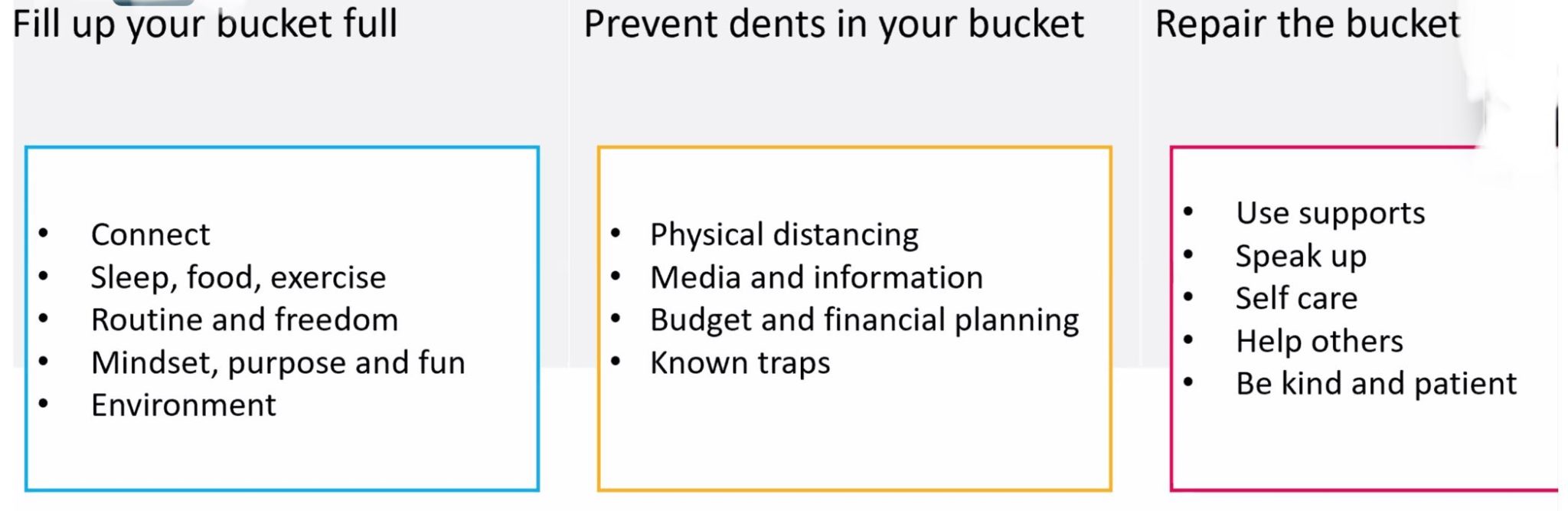
To support business owner, Beyond Blue has co-created a program “NewAccess” for small business owner. There are a number of other resources for small business as well as for individuals.
For small business
For individuals
At Geelong Chinese Medicine Clinic, we find that the common physical symptoms brought on by or worsened by mental health are bodily pain, disturbed sleep, fatigue, mental fogginess, digestive issues, skin issues, and menstrual issues for females. If you suffer from those symptoms, please ensure you consult your family doctors to check out and reflect on any mental stresses you might have. You are most welcome to consult with our practitioners.
Let us use this difficult time to turn our focus to mental health and build awareness and resilience.
It is commonly known that weight gain occurs when there’s an imbalance between energy intake and expenditure. But how do we see weight gain in Traditional Chinese Medicine (TCM)?
There are four main reasons to gain weight from the TCM perspective (Li, 2014) :
Firstly, heat in the stomach combined with poor digestion due to improper dietary habits and lack of exercise (Li, 2014).

Secondly, Qi, the vital energy, stagnates due to emotional disturbance, which impedes digestion, and slows down the bowel motion, causing fat accumulation (Li, 2014; Maciocia, 2005).

Thirdly deficiency of Yang, i.e., deficiency of the fire, in the body causes weight gain (Li, 2014; Maciocia, 2005):
Finally poor digestion, long-time sitting and improper dietary habits, can form dampness or make the body “soggy”, and eventually turn into fat (Li, 2014; Maciocia, 2005).


So the take home messages are:
In our next blog, we will talk about the Chinese medicine treatments and suggestions for weight loss. Stay tuned!
References
Li, K. (2014). Efficacy and safety of Chinese herbal medicine and acupuncture in the management of obesity: Systematic reviews and a randomised placebo-controlled clinical trial (Doctor of Philosophy Dissertation), RMIT University, Melbourne, Australia.
Maciocia, G. (2005). The foundations of Chinese medicine: a comprehensive text for acupuncturists and herbalists (Vol. 1).
Figures are obtained from https://www.facebook.com/115900903536977/posts/135919798201754/
Geelong has experienced a few lockdowns in the last 18 months. Many of us have been working or studying at home; and some have gained weight during those lockdowns. At the same time, a large number of us experience stress and poor sleep during. In the PhD thesis (Luo, 2021) written by Dr. Rose Luo, one of our practitioners at Geelong Chinese Medicine Clinic, she explained how these three health issues are linked. We here share the findings.
Stress is one of the contributing factors of weight gain:
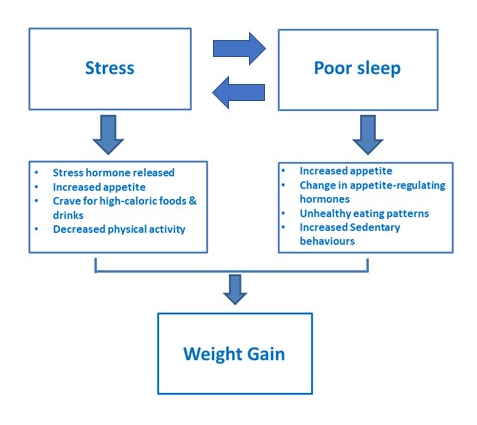
Poor sleep with shortened sleep hours also leads to weight gain:

So poor sleep, stress and weight gain are closely connected and creates a vicious cycle. In the next blog, we will talk about how Chinese medicine understands weight gain; and how it might help with breaking the cycle.
References
Luo, S. (2021). Development of a weight-loss product using Chinese herbal medicine combined with nutritional technologies (Doctor of Philosophy Dissertation), RMIT University, Melbourne, Australia.
Reutrakul, S., & Van Cauter, E. (2018). Sleep influences on obesity, insulin resistance, and risk of type 2 diabetes. Metabolism, 84, 56–66. doi:10.1016/j.metabol.2018.02.010
Tomiyama, A. J. (2019). Stress and obesity. Annual Review of Psychology, 70, 703–718. doi:10.1146/annurev-psych-010418-102936
Have you found sometimes a delicious dinner makes you feel great at that time, and you still feel great the next day; whereas other times a lovely meal makes you feel good at that time but you feel terrible the next day. Similarly consuming some food might worsen your pain; whereas others lessen pain.
At this year (2021) Australian Pain Society Conference, a special workshop on diet and pain was presented. We were told that there is up to 2 kilograms of gut bacteria in our body, some are good and some are bad. All of them are closely related to our diet, and impact on not only our digestion, but also
At Geelong Chinese Medicine clinic, we are often asked what kind of food is bad or good for pain. A recent systematic review (1) examines 44 eligible clinical trials on diet and pain, including patients with rheumatoid arthritis, fibromyalgia, osteoarthritis, other musculoskeletal pain or neuropathic pain. The review looked into vegetarian/vegan die, single-food changes, elimination protocols, energy and/or macronutrient restriction, focus on omega-3 intake, or a Mediterranean diet. About half of the studies reported reduction in pain as well as positive metabolic changes. Overall whole-food diets are linked to positive changes in pain, regardless the types of diet. So it comes down to the quality of food and nutrient intensity.
Because pain has a close relationship with our mood and body inflammation, any food that could impact on those two will have either positive or negative influence on our pain. The table below illustrates the types of food to have or avoid to decrease inflammatory load in our body, therefore potentially reduces pain (2,3).
| Food to avoid or reduced quantity | Food to have |
| Processed food | Whole food, particular fruit, vegetables |
| Food with high glycaemic index, e.g., white bread, corn flakes, watermelon | Low glycaemic index: e.g., multi-grain bread, oats, apple |
| Nutrient poor | Prebiotics and probiotics, e.g., whole grains, legumes, tomatoes |
| Saturated fats, e.g., butter, coconut oil | Unsaturated fats, e.g., sardines, walnuts, olive oil |
| Overeating or fasting | Balanced eating |
Advice on food, what is good for us and what is bad for us, seems to change all the time. One minute we are told red wine is good; and the next any alcohol is bad for us. One minute butter is bad, now we are told that butter is good. We can see this change negatively, reflecting that experts know little; or see this change positively, that experts rely on science and evidence to guide us on what, how and how much we should eat.
A few weeks ago, I attended a seminar delivered by a leading expert on Mediterranean diet (Med Diet), Professor Catherine Itsiopoulos, the new Dean of the School of Health and Biomedical Sciences at RMIT University. The Med Diet has been very popular in Australia. Prof Itsiopoulos’s talk was very enlightening. I had a few of lightbulb moments.
Prof Itsiopoulos says that true Med diet is a “peasant diet” with little meat, not the ones featured in some Med diet cookbooks where festival food is promoted. The pyramid below highlights the key features of a healthy Med diet.
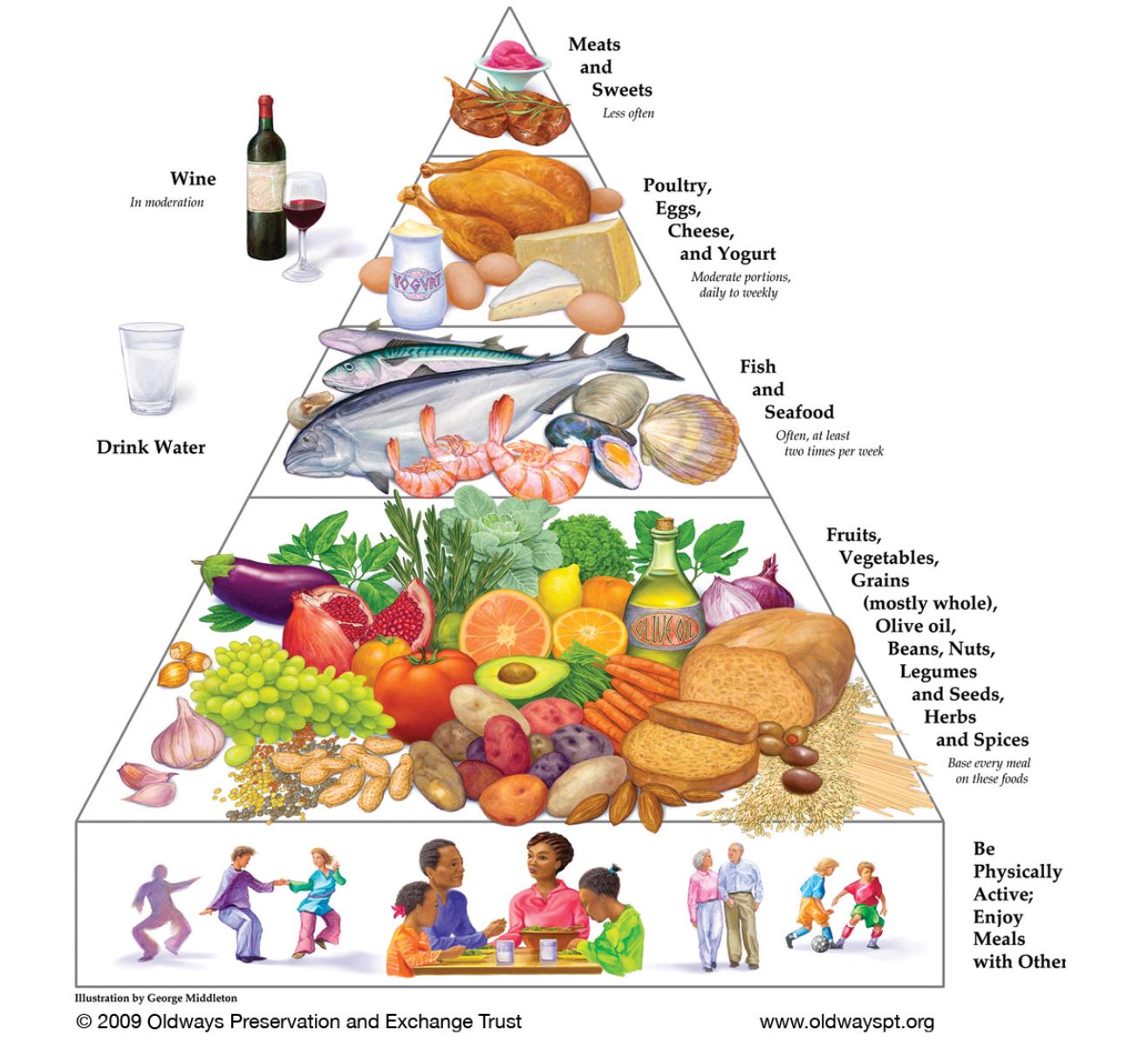
In summary, varieties, whole food, eating with friends or family, planting or cooking our own food, and reducing or removing snacks are the keys for successful and healthy diet. Diet is about food, as well as about everything around food and eating.
Further readings:
Note: This book is specifically written for Australian Audience. pp224.
There are many factors can affect the skin health. Traditional Chinese medicine (TCM) believes that facial complexion and the skin are reflections of the function of the internal organs. For instance, a pale complexion or dry or prematurely aged skin reflects the internal disharmony, such as digestive intolerances, hormone changes or oxidative stress.
Our internal status is affected by seasons, environmental factors, our emotion, lifestyle an / or pre-existing diseases; therefore the skin health is also impacted by those many factors.
We know that a dry or hot environment can dehydrate skin, leading to dry or aging skin. Such dryness in Chinese medicine could be related to the Lung. So people with chronic respiratory conditions often has dry skin and pale complexion. Constant anxiety or fear often leads to drier and darker skin, in particular under the eyes. Anger or excessive consumption of alcohol builds up heat in the body, and disturbs the Liver in Chinese medicine, which leads to pimples or skin rashes. Poor diet with frequent consumption of fast food, or worrying and overthinking, interferes with nutrient absorption, leading to a sallow complexion and tired looking skin.

So skin health is really an inside out issue. To rejuvenate skin health, we must use Chinese medicine diagnostic skills and knowledge to identify and assess any internal imbalance within an individual, explore potential causing factors, then develop treatment plans to address those internal disharmonies. At the same time, we will apply therapies to the skin and face to address the external appearance and skin health.
To improve skin health, at Geelong Chinese Medicine Clinic, we commonly use facial acupuncture, body acupuncture, and facial massage. Additional medicinal herbs can be used to address more severely version of internal disharmonies. Of course we will provide personalised advice to improve general health ad wellbeing, as we know skin is a business about inside out.
In our previous blog, we talked about mid-life transition. In women, this transition is obvious as menstruation starts to become irregular. The average age for this transition is about 47 years old, and this phase may last for 4 years. People are familiar with hot flushes and night sweats, however changes in sleep and mood during this stage are extremely common, yet less talked about. About one in two women during peri-menopause experiences sleep disturbance or insomnia, and 25% to 45% suffer from anxiety or depression. Women in their 40s and 50s are often the key contributors to the workforce and family life. Increased responsibilities, lack of sleep and mood issues significantly impact on the quality of life of women in this age range. In Geelong, over 30,000 women are in their 40s and 50s.
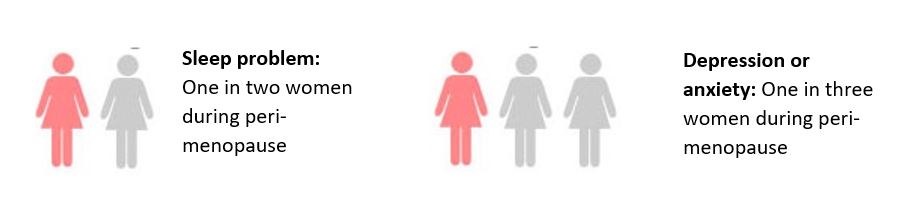
Sleep deficiency greatly impacts on mood. Yet mood may worsen sleep. Various menopausal symptoms impact on each other and create a vicious cycle.
Hormonal replacement therapy, melatonin, hypnotic medications and anti-depressants all have their places, but not without side effects. Cognitive behavioural therapy is found to be effective to address sleep and depression for peri-menopausal women.
Acupuncture is anther non-drug therapy that has shown promising results in improving hot flushes, night sweating, sleep disturbance and mood changes. Utilising the holistic theory of Chinese medicine, practitioners develop different acupuncture plans to address a number of menopausal symptoms simultaneously, yet with a focus on a couple of key issues.
In addition to providing acupuncture and / or Chinese herbal medicine treatment, we encourage women to adopt some self-care approaches, which aim to provide sustained results. Those strategies include
The overall aim is not only to help smooth the life transition, but also to build a strong foundation for the years to come.
Cannot fall sleep at night, frequent waking up, or waking up at 1 or 3 o’clock in the morning? You are not alone. Based on a 2019 Sleep Health Foundation report that at least one in two adult Australians experiences one of the above mentioned sleep problems three or more times per week; and one in six adults could be diagnosed to have chronic insomnia. Sleep problem occurs in all age groups, but is more common as we get older. Women are more likely to experience sleep disturbance than men.
Insomnia or sleep disturbance is one of the commonest symptoms we see at Geelong Chinese Medicine Clinic. Yet most people do not come for help with their sleep issue. People often come because of low energy, foggy brain, digestion issue, pain in the body, blocked nose, anxiety, skin problems or other issues. Sleep issue is only identified after our comprehensive inquiry. So sleep problem or insomnia is under diagnosed and consequently under-treated. Research shows prolonged poor sleep is linked to poor quality of life, depression, anxiety, chronic pain, diabetes, obesity, cardiovascular diseases, such as hypertension, heart attack, and stroke, and even dementia.
Luckily, no matter what causes sleep disturbance, there are something everyone of us could do. It is called sleep hygiene. It is effective. For some people, observing sleep hygiene is sufficient to improve their sleep, whereas others also need professional help. Please make sure you check out the link for excellent information.

Chinese medicine considers two important factors for a good sleep:
Below is a list of the common mistakes we see in our patients. Check if you have any of them.
Table: Some activities to be avoided or encouraged before bed.
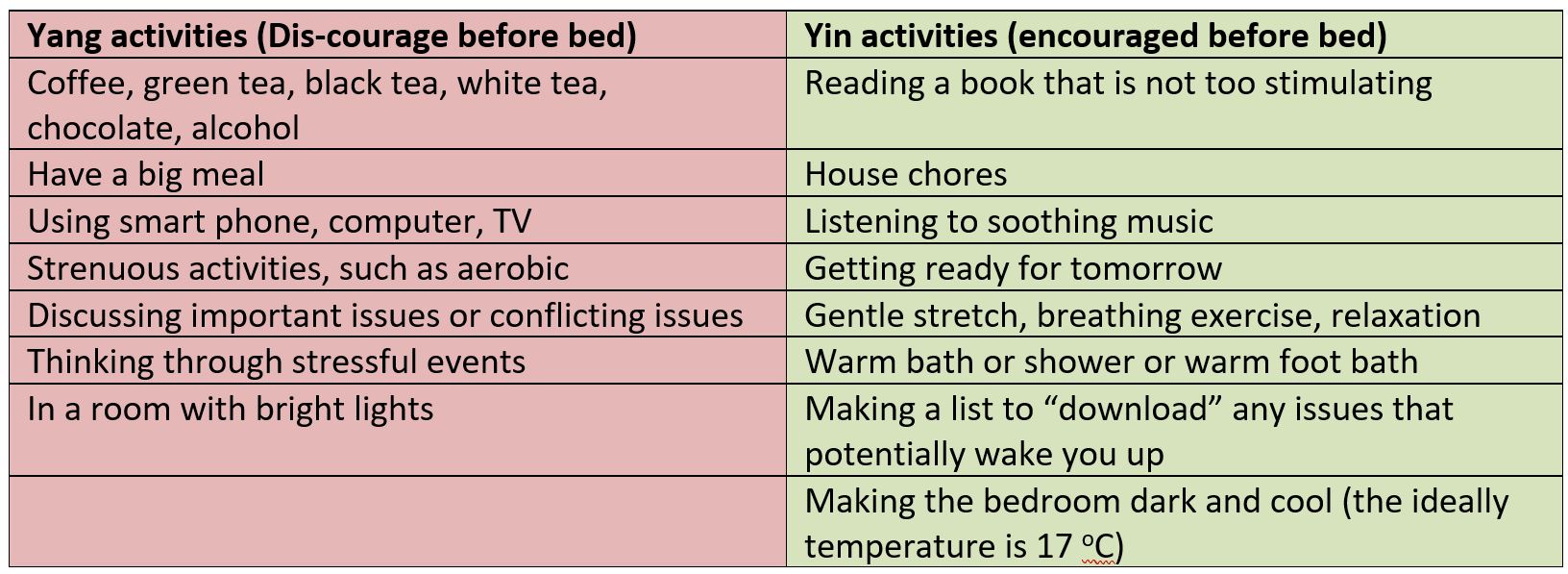
I attended a seminar last week about mid-life wellbeing. The middle-age individuals are those between 45 to 65 years old. Mid-life is the phase when one faces physical, mental and societal challenges. The top health issues during this phase are reduced immunity, weight gain, fragile bones, and increased incidence of cancer. On the one hand middle-aged individuals are no-longer as energetic as they were in their 20th, on the other hand they have more responsibilities and stress at work, and at home due to having children and ageing patients.
We see many middle-aged people in our practice in Geelong. Most of the complaints are related to fatigue, sleep disturbance, digestive issues, stress, bodily pain, headache, sinuses infection or menopausal for women. Those physical symptoms reduce people’s capacity to cope with the increased pressure and stress.
In addition to family and societal demands, middle-age individuals decline physically due to the change in body essence (Jing). In Chinese medicine, Jing is what we are born with, and inherited from our parents. It is called pre-natal Qi, which governs our growth, maturity, fertility and longevity, and is the foundation of our health. Jing is weak when we are born, and grows as we grow, reaching its peak around late 20th and early 30th. From there, Jing declines. During middle-age, there is a sharp decline. The body’s capacity to adjust to changes could not catch up with the speed of decline, leading to many symptoms. After that, Jing continues to decline with a gentler speed as shown in the figure below.
This seems to be a doom picture, that we are getting weaker after 35 years old. Well the body is so amazing, it always has multiple backups. According to Chinese medicine, Jing is be supplemented by post-natal qi, which refers to the energy created by us after we were born.
This is a great news for those who are middle-aged. So there are ways to strengthen Jing when it is naturally declining.
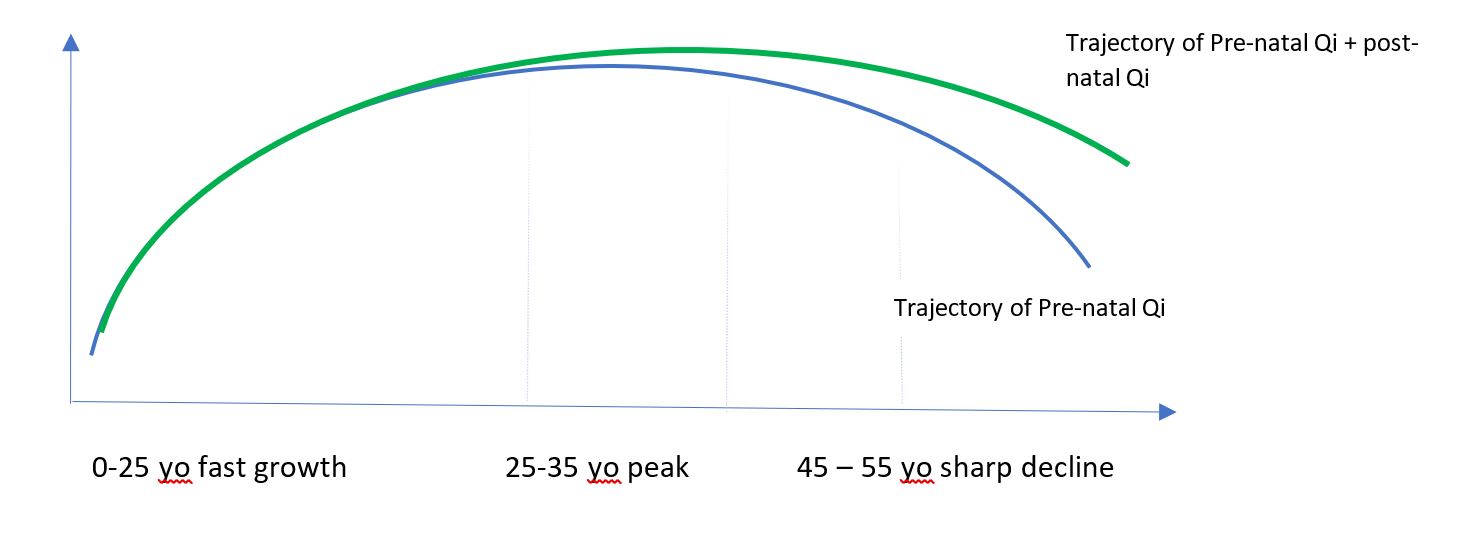
Ways to strengthen Jing are simply, and do not cost much. All you need is to be consistent and persistent.
As you can see there are so many simple ways to supplement our declining Jing.
Middle-age individuals are in the most important phase in life. During mid-life, we tend to put ourselves the last due to so many competing duties. Now it is time to give ourselves TLC to set up a great foundation for a successful ad healthy ageing. Research shows if we adopt those good habits in mid-life, we will enjoy extra disease-free years, with 7.6 years for men and 10 years for women. Let us turn “mid-life crisis” into “mid-life opportunities”.
Spring is here. Today Geelong is nicely warm, a perfect spring day.

You might have dusted your house, weeded your garden to welcome the spring. This morning my Qi Gong instructor reminded us to also spring clean our body. His comments inspire me to write this blog.
From Chinese medicine point of view, Spring is the time for growth and is dominated by wind. We are part of the nature. The change of seasons also brings changes in us. The arrival of spring might make you wanting to be outdoors, and to be active. Those are positive aspects. The energy however that encourages growth also stirs up what is in dormant, like the hurricane bringing up dust and everything in its path.
So how do we know if we have issues need to be “spring cleaned”? Here are a few signs.
So how do we spring clean our body?
In Chinese medicine, mind and body are closely linked, via Qi. That is how emotional issues are manifested through our body, and disturbance in our body can cause disturbed mind.

So spring cleaning the body is to spring clean the Qi to help your body reach a balanced state. Here are a few strategies:
When the house is dusted, garden is weeded, it is time to declutter our body.
Nowadays, many of us work or study from home. Prolonged stay in a cold room has the similar effect on our body as being in a cold outdoor environment. Coldness can damage vitality of our Qi. When the vitality is impacted, we feel fatigue, sleepy, hungry or pain or stiffness in some parts of your body. We may or may not feel the cold. More and more people come to our Chinese medicine clinic in Geelong for those signs and symptoms.

There are two guiding principles to prevent your body from being harmed by the coldness.
Outdoors in a winter is an obvious cold situation. This is not the only time when one is exposed to the coldness. Many of us work or study from home. Most of the Australian houses are not well insulated, so indoors can be cold. Sitting at the desk or in front of a computer for too long allows coldness to impact on us. In summer, coldness also happens as conditioners blow out cool air constantly.
Here are TEN tips to prevent coldness from impacting on you

Stay warm, staysafe, and stay well.
The Taiji (Tai Chi) Qigong Shibashi (18 movement)
is a modern Qigong form combining elements from the Yang form Taiji and more traditional breathing and movement exercises from Qigong. The routine combines slow, deliberate movements, meditation, and breathing exercises and can be done in one place (standing or seated). It is an excellent gentle exercise activity for beginners and people with health conditions.
A link is provided below for a follow-along video demonstration of Shibashi (filmed in mirror image by Geelong Chinese Medicine Clinic’s registered acupuncturist & herbalist and qualified Qigong instructor Paul Burns )
While the routines are not high intensity they are designed to help:
One of the best features of Tai Chi and Qigong is that they can be adapted to fit just about any fitness level. Yes, you can modify/ shorten repetitions or not do the movements if they are not suited to your body/ injury. While the breathing & movement coordination is not described in the video, just go with what feels natural such as inhale on the lift / expand movements and exhale on the body contract / descend movements (Please stop if at any time you feel dizzy). As a beginner don’t stress yourself co-ordinating the breathing and movements, and always return to natural breathing if needed. The gentle, low-impact flowing movements are easy on the joints. You can even do the movements seated. Simply doing the gestures as a gentle exercise will bring about positive results, but it becomes more of Qigong when the person practicing becomes more actively aware of the mind and breath with the movements.
But check with your doctor first if you have any conditions such as:
To see the follow along online video of the Taiji Qigong Shibashi click this link Taiji Qigong Shibashi
We are facing a pandemic. As of 1 April 2020, the city of Great Geelong has 43 cases tested positive for COVID-19. When facing the same viruses or pandemic, some people are affected badly whereas others do not suffer from many signs and symptoms. A healthy body system is often the reason behind. The people are affected the most b COIVD-19 are the older people over 70 years, people who have pre-existing conditions, such as asthma, heart disease, diabetes, or people’s immunity is comprised due to chemotherapies, organ transplants etc.
In Chinese medicine, disease occurrence is the result of the fight between Righteous energy, or factors (Zheng Qi) that protect and support us to heal, and Evil energy or factors (Xie Qi) that try to invade our body and conquer us. When Righteous Qi is strong, one may be able to prevent the Evil Qi entering into the body or minimise the impact of Evil Qi. Righteous Qi is not simply equal to Immunity. The fight between Righteous Qi and Evil Qi is similar to the fight between Obi – Wan Kenobi and Darth Vader.
To ensure we are healthy, in particularly during a pandemic, it is essential we maintain strong Righteous (Zheng) Qi. Knowing the factors impacting on Zheng Qi will help us develop good strategies.

We will discuss each factor and what we can do to strengthen our Righteous Qi (Zheng Qi) or defence in blogs of the coming weeks.
To support government effort to curtail the spread of coronavirus, we will temporarily suspend face to face consultation and acupuncture service from Mon 30th March. We will re-assess the situation week by week.
Let us work together to combat the pandemic.
Geelong Chinese Medicine Clinic wishes you well and safe during this difficult time. Remember to be gentle to yourself and to your family.
We talked about Qi Gong on our website. Qi Gong is a form of exercise and self-care, and similar to Tai Chi, but it is gentler and is suitable for most people. There are many benefits of Qi Gong, including calming and enhancing the immunity. Please read our previous blogs on this topic and relevant research.
Here is a short Qi Gong session of 18 min that is specifically recorded by Master Liu to help people breath more deeply and strengthen the immunity. Master Liu is the 5th generation inheritor of the Liu He Zi Ran Men lineage. He has 30 years teaching experience in China, Australia, Europe, and South America. He combines his expertise in Qi Gong tradition with knowledge of modern science, Eastern and Western culture, in his teaching of Qi Gong.
Two staff members of Geelong Chinese Medicine Clinic, Paul Burns and Zhen Zheng, train under Master Liu. In March 2020, Paul received his Master Instructor certificate and Zhen received her Level 1 instructor certificate.
Key points of this Qi Gong session
Important message
Please prioritise self-isolation and hand hygiene. No other preventive measures work better than self-isolation and hand hygiene during a pandemic like COVID-19. Let us remember those hospital staff who risk their safety to stay at work. What we can do is to stay at home to help them and to break the chain.
Video: Qi Gong to strengthen the immunity and keep you calm

In the last post, I talked about awareness. Here I introduce some practice to gain better awareness.
Recently I had the opportunity to attend a Qi Gong training in north NSW delivered by Master Liu (Deming) from China. The theme of the training is called Qi Gathering, and I call it a new way of moment and connection; or a way to awareness.
The essence of this new way is Relaxation creates Space, Space creates Qi, and Qi creates Movement.
We know usually movement starts with an intention. We want to walk up hill, we want to stay upright, or we want to jump. This intention creates muscle contraction, to prepare us and to propel us to move. Then bending a knee and raising a foot to walk uphill, or contracting muscles of the back to stay upright, or bending the knees to push upwards.
In Qi Gathering, movement starts with relaxation but not an intention. I called it a new way of movement. It might NOT be new to some people, but will be to many. This involves emptying the mind and relaxing the body, which allows a space to be created, but not to be occupied with an intention, a thought or a desired outcome. In this space, Qi is created and so is the movement. This is similar to the breeze passing through a room when a door or window is open. This form of passing through, like breeze, is the movement.
Experiment this. Now stay upright with your usual way and close your eyes. Now feel where you feel the tension and tightness. You might feel it in the low back, in the neck, in the abdomen, in the legs or in the feet. Now try again, only this time, you envision you feet planting on the ground, you relax your whole body and you relax your breathing. As you relax, you create an awareness of a space above you. This space creates Qi with a gentle uplifting force. This Qi guides you to stay upright. Now check yourself again. You will find you are staying tall and upright. Yet you do NOT have any tightness you felt the previous time. Instead you are staying upright, tall, effortless and light.
This is the foundation of Qi Gathering. Regulating Qi is the foundation of acupuncture or Chinese medicine. If you can feel what I describe here, then congratulations. This means you have a great awareness of your body, and mind; and the great ability of letting go. If you could not feel what I describe here, then please do not get worried. If you want to experience this effortless movement, you may want to start some Qi Gong training with a teacher.
This form or concept of movement will help reduce injuries and bring agility into your movement. More important, it will bring awareness into our body as we go through our daily movement. This is mindful movement.
One could easily apply this principle to relationships with oneself or with others. The essence is letting go creates connection. We can expand this in future blogs.
Please have a look at these two short videos about Qi Gong in Geelong.
Basic Tai Chi Standing Posture
Tai Chi / Qigong Gentle Warm Up

In our previous blog, we discussed what a balanced state looks like. This help you understand when you are balanced and when you are not balanced. In our Chinese medicine practice, people often ask us what they can do to create or maintain a balanced state. We are often overjoyed to hear this question. This question indicates that the person has made the first most critical step to a balanced state as the person has made the task their responsibility. Indeed, a Chinese medicine practitioner may help you create a balanced state, but this state relies on the person to maintain.
A balanced state in Chinese medicine means “Yin is calm and Yang is securely inside the body to drive the life force”. That is to carry out daily activities and tasks in a calm status with direction and clear awareness.
They are ways to carry out each strategy. In this blog, we will focus on how to be aware.
Often we go through life with little awareness of our thoughts or our emotions as we are busy in carrying out the conversations inside of our head. The next minute we know we are angry with some remarks or we are upset for ourselves or others not doing things properly. Those are the imbalanced moments. Actually way before those upsetting moments, dis-comfort has been simmering. If we detect those, we could easily dis-engage at that time and prevent later upsets.
To be aware, one must maintain mental clarity, including sleeping well, eating a balanced diet, and engaging in daily physical activities and awareness training. To learn how to be aware, we highly recommend reading some books or learning some techniques. There are many good resources. Here are just a few.

Qigong vs. Tai Chi
Qigong and Tai Chi (Taijiquan) are two forms of ancient Chinese exercise for health. Tai Chi is well known in Geelong, however many people are not aware of Qi Gong and do not know the difference between the two. In this blog, we give a broad overview of similarities as well as differences.
Qigong (roughly translating to energy exercises, or Arts of Qi) is an inclusive term to describe exercise practices that focus on cultivating the Qi, or internal energy, to improve health, fitness, wellbeing and longevity.
Tai Chi (developed later on) was a form of martial art developed with Qigong understanding of internal energy and how to use it for health or fighting. Tai Chi in the modern days is mostly practised with a focus on its graceful Qi cultivation side for health rather than for combat.
Qigong and Tai Chi both have been developed from the same concept of Qi that is emphasised in Chinese medicine and acupuncture. Qi gives energy to life and the fluent and constant flow of Qi through the body helps maintain our health. When the flow of Qi becomes stagnant or blocked, illness can occur.
Similarities:
Qi Gong & Tai Chi share the following similarities:
Differences:
They differ in how they are practised and level of difficulties.
Application and practice
Level of difficulties
In closing both Qigong and Tai Chi are good for health. They complement each other, and are often taught together. If anyone is interested in experiencing these health practises please click on the link Qigong for more information.

Following from our previous blog on what balance means, here we discuss what a balance state looks like. A balanced state is the natural state of our being. It is a state Chinese medicine described as “Yin Ping Yang Mi”. It means Yin is calm and Yang is securely inside ourselves to drive the life force.
This is an important question. If we do not know or experience the balanced state, then we will not be able to detect when our system is off balance. Here are a few key experiences.
Being balanced does not mean someone is in a total blissed state all the time without upsetting moments. Remember the Yin and Yang balance is dynamic. If you are upset, a balanced state means you will not stay in the upsetting situation for long. You are there for a few minutes or one hour or a few. You will not spend days or weeks on the same upsetting situation.
How does one stay in a balanced state or learn to be balanced? We will discuss this in future blogs. One of the methods that can be adopted by anyone is Qi Gong, or the arts of Qi (chi). It is a form of slow movement combined with breathing, mindfulness and slow stretching. Please read our blog on this.
During the long weekend holiday a couple weeks back, two staff members from Geelong Chinese Medicine Clinic, Paul Burns and Zhen Zheng, as well as Geelong psychologist Helen Handsjuk, went for a Qi Gong retreat. We had lots of training on how to be centred or balanced with Qi Gong. Paul received his certificate for Level Two instructor and Helen received her certificate for Level One instructor. Well done, and congratulations to both!

(From left to rigth: Paul, Helen, Master Liu and Zhen)

Healthy eating is very important. The types of nutrients in the food we consume determine the composition of every single cell in our body. On average, an adult loses roughly 300 million cells every day and we are replacing them with food. Our bodies are literally manufactured out of food we eat.
Chinese medicine understands that food has different nature and different tastes. “We are what we eat” means our constitutions are closely related to the food we choose to eat. Choosing the suitable food can improve our constitutions, or our potential to remain healthy. Here we discuss a few common types of diet and related patterns of body constitutions and provide advice on how to improve if one wishes.
The “Damp” person
Those who love high fat and high carbohydrate food would usually feel heavy in the body, and cloudy in the head. Those symptoms get worse in the afternoons. This presentation in Chinese medicine is called “dampness” accumulation in the body. Then how to get rid of “dampness”, and feel lighter in the body and clearer in the brain? Here are some tips:
The “Hot” people
“Hot” here does not really mean popular. Australia is a red meat consumption country. In Chinese medicine, eating too much red meat will produce too much heat in the body. Red meat lovers usually have red cheeks, are less tolerant to heat, feel hot and sweaty easily and crave for cold drinks. These symptoms will subside once red meat is reduced from the diet.
The “Blood” weakness type
Vegetarian and vegan diet or people who don’t like eating much meat tend to show “blood” weakness in Chinese medicine. Blood weakness is not equal to anaemia. Those people may have pale complexion, experience dizziness or low energy or feel cold in the hands and feet. They are recommended to take less raw or cold food and drinks. Replacing salad with steamed vegetable and having soup more often could be a very good start.
A healthy diet in Chinese medicine is a balanced diet, is eating many varieties in a small quantity. Whole grains, meat (red or white), vegetables and fruits, natural, seasonal, whole food and food of different colours should be included in our everyday diet. It is recommended to take at least 20 different types of food every day. In Geelong we are fortunate to have access to fresh, local and varieties of food. Let us make good use of that.


Patients often ask us at Geelong Chinese Medicine Clinic what they can do at home to aid in their recovery or maintain their health. Along with diet, the movement based Qigong (See Qigong under Services heading for further explanation) exercises are the most practical for patients to do at home. Qigong exercises involve slow and gentle body movements with deep breathing and mindfulness. They are easily learnt and can always be modified based on individual’s ability or injury and illness.
Available to Chinese medicine are many medical and health-promoting tools such as Acupuncture, Chinese herbal medicine, cupping, moxibustion, massage and food & diet therapy. Included under this umbrella are the self-health exercises of Qigong.
Qigong for health maintenance and healing has long been used throughout Asia, and one just has to stroll down to any city park in the early morning in China to see the population’s belief in self-health maintenance exercises.
Modern scientific understanding of our bodies confirms what we already know,
Here are the obvious advantages of Qigong exercises:
Including Qigong exercises in your life is an easy way to help maintain a balance of the body and mind.
Paul teaches Qigong through Geelong City Yoga with Geelong psychologist Helen Handsjuk on Wednesday AM and through Geelong West Neighbourhood House on Thursday evening.
Are you familiar with this symbol? Of course, you say, who does not know?

But what does it mean? And how is it related to Chinese medicine?
This symbol represents the essence of the Theory of Yin and Yang, which is a philosophical understanding of the world, and is also the foundation of Chinese medicine. When Chinese medicine says Balance and Being Holistic, it refers to the Balance of Yin and Yang, and Yin and Yang together being the oneness.
This symbol says
That is Yin and Yang complements each other, and inseparable.
Yin refers to the moon, water, being cool, being statics, female, quiet, and slow; and Yang refers to the sun, fire, hot, dynamic, male, loud and quick. From health and illness point of view, a condition that is cold in nature and gets worse with cold weather or environment, it is Yin in nature. Fever, or being thirty, is considered of Yang in nature. Every phenomenon can be understood as Yin or Yang; yet in every phenomenon there are Yin and Yang elements.
When Chinese medicine talks about Balance, tt is the Yin and Yang elements that need to be balanced.
Being balanced is the ultimate natural stare of the universe. When this balance is out of its order, that is when illness happens in humans. As you can see in the diagram, the balance is not 50% vs 50%. It is a dynamic balance because the components of Yin and Yang change over time and all the time. Morning becomes noon, noon goes into afternoon, which then becomes night; night will go into dawn. This cycle continues, as Yang (morning and noon) goes into Yin (afternoon and night), and goes to Yang again. This is the dynamic balance of Yin and Yang.
Everything in the Universe consists of Yin and Yang; we are part of the Universe, so we human beings too have Yin and Yang within our body. Any external Yin and Yang changes will impact on our internal Yin and Yang. This explains why weather could impact on us. For instance in the last a few days, Geelong has been very hot. We too feel the heat. For instance before the rain comes, those who have arthritic joints will know due to a change of air pressure from high to low (from Yang to Yin). This explains oneness of our body with the Universe.
Chinese medicine positions itself on Yin and Yang theory, and considers human beings are one part of the whole Universe and follow the same rule that regulates the Universe. That is why Chinese medicine considers all most everything that is NOT balanced could impact on our internal balance and become the cause of diseases. To become healthy again, one needs to regain this balance. To prevent one from being ill, it is essential to keep yourself Yin and Yang balanced so that this natural status will not be swayed easily by things that are out of balance.
In the future blogs, we will discuss what are considered causes of diseases and how to recognise them. And what we can do to maintain the natural state of balance.

Summer is here, and will be here for a while. In Geelong, summer can be hot, humid, and the temperature also changes dramatically, varying from 42 degree to 20 degree within one day.
When hot, naturally people want to take cold food and cold drink to help with the heat or dress coolly, such as wearing saddles, vests etc. In Chinese medicine, this is however a poor practice. Coldness is one of the major causes of health conditions in Chinese medicine. In winter, we dress warmly to cope with the cold, but in summer we forget that there are also cold factors when the day temperature drops greatly or when the sea breeze comes through at night.
In fact, summer is the main season when the cold environment or cold food impacts on us quietly, such an impact could show immediately, but more often the impact won’t show until winter. If you suffer from cough or asthma in winter, if you have stomach pain, diarrhoea or abdominal bloating easily, if you suffer from painful periods (for girls), or if you have low back pain or arthritis, keeping yourself warm is particularly important in summer. Those conditions indicate you are prone to be affected by the cold environment or cold food. At our Chinese medicine clinic in Geelong, we identified some commons causes leading to coldness invading into the body, and have generated a list of tips to keep yourself warm in summer and prevent from health problems in winter.
Tips to prevent coldness invasion in summer
• Take warm drinks, such as tea or coffee or warm water. Do you know taking warm drinks actually help cool your body? This seems to be counterintuitive. Check out this article.
• When eating cold salad or food, make sure you also eat something warm or drink something warm at the same time to reduce the impact of cold.
• When going into a room or place that is air conditioned, for girls or ladies, please bring a shawl to cover your shoulders; for gentlemen, please wear short or long sleeve shirts, but not vests. This is particularly important if your office is cold. You could be exposed to a cold environment for 8 hours straight. One of my common “prescriptions” is a few beautiful shawls for ladies.
• When sleep, make sure you are covered with something; even a thin sheet would be very helpful. Our body temperature drops when we sleep or be in station and this is the time when a cold environment impacts on our body greatly.
• Sitting or sleeping away from any direct wind. Wind helps the coldness penetrate into the body.
So food, drink and dress are the ones to think about in summer.
![3[2]](https://www.geelongchinesemedicine.com.au/wp-content/uploads/2018/11/32.jpg)
The Traditional Chinese medicine (TCM) team at Geelong Chinese medicine clinic (GCMC) welcomes you to spring. As acupuncturists and Chinese medicine herbalists, we see numerous people suffering from seasonal and all year round allergies. Along with conditions such as pain, headaches, migraines, anxiety and depression, allergies are one of the most common conditions seen in our clinic.
If you suffer from Hayfever/ seasonal allergic rhinitis (SAR), basically it involves the body’s immune system becoming over reactive to certain things in the environment (i.e. pollens) that aren’t a problem for most people. There are many theories on the different ways that cause this, but simply your body has learned to be allergic to certain things.
Hayfever (SAR) symptoms: (similar to cold or flu like symptoms)
Modern allergy medications for Hayfever (SAR) come in various forms such sprays, tablets, syrups, flushes and even injections to provide short-term relief. They do not cure allergies, but simply block the symptoms.
Are there natural alternatives to help stop or reduce the need for allergy medications for Hayfever (SAR)?
This is a common question from patients at Geelong Chinese medicine clinic.
The short answer is yes.
Traditional Chinese medicine (TCM) offers both acute symptom relief management and longer period treatment to attempt to regulate the TCM constitutional imbalances and calm the immune system overreaction.
A 2018 clinical trial review of acupuncture on antihistamine use in patients suffering seasonal allergic rhinitis showed the acupuncture group had a lot fewer days (10 days less) of antihistamine use and 38% of the acupuncture group didn’t need any medication at all in comparison to 16% in the routine management group (Adam et al, 2018)
Best time for treating Hayfever (SAR)
Just like preparation for bushfires is best done before the actual fire season, in regards to Hayfever (SAR) the best time to come for treatment is 2-3 months (Autumn/Winter) before the hayfever season (Spring) starts. For all year round sufferers, anytime is a good time to start treatment.
But as most people don’t know this, the majority of Hayfever sufferers come in peak season (Spring). When this happens we end up focussing more on symptom relief before we can get to working on underlying constitutional causes. However, we aim to lessen their symptoms and then decrease allergic responses in following seasons.
Future Blog articles will address self-care strategies for Hay fever/ SAR sufferers such as commonly used acupressure points that can help reduce acute symptoms.
References:
https://www.ncbi.nlm.nih.gov/pubmed/29440045
The views on healthy food change all the time, usually depending on the latest research findings. In Chinese medicine, the concept of healthy eating has never changed. Choosing from seasonal and unprocessed food with various colours and flavours to match with individual constitution is the key of a healthy diet. In Chinese medicine, food is considered as important as medicine.
Indeed, we are what we eat!
Same as Chinese medicine herbs, food have different natures: cool, cold, neutral, warm, and hot. The nature of food is determined by the effects they have on the person’s body after consumption. If a person frequently eat the same type of food, it creates imbalance in the body. For example, red meat lovers usually show excessive heat in the body, with symptoms such as feeling hot, sweaty, thirsty, grumpy, and constipation.
Food is also categorised by their taste. There are five different tastes: sour, bitter, sweet, pungent and salty. Each taste of food corresponds to a different organ in Chinese: sour food enters the Liver, bitter food is good for the Heart, sweet food strengthens the Spleen, pungent food nourishes the Lung and salty food goes to the Kidney. Here Liver, Heart, Spleen, Lung and Kidney refer to Chinese medicine organs, but not those of Western medicine.
The climate is an important factor of our food choices. People from hot and humid places will benefit from eating some spicy food to bring sweat out (to remove dampness from body). Whereas in Geelong, it is dry and windy in most time of the year, residents are recommended not to have too much chilli and spices, but eat more seasonal vegetables and take more soup and broth to reduce the impact of the dry environment.
Remember it is all about balancing and nurturing the body.
Reference:
https://www.dw.com/en/healthy-eating-in-traditional-chinese-medicine/a-18619239
Spring is coming. Sunshine, green grass and flowers. Life is beautiful again, although that may not be so to some people. With spring, here comes hayfever. If you have an itchy nose, runny nose, and/or itchy eyes, and sneeze a lot, then you might have hayfever, which is also called seasonal allergic rhinitis. For some people, the symptoms are so bad that their sleep is disturbed and their physical and mental functioning decline because the nose is so blocked.
It is easy to take antihistamines, but for some the medications do not work, or used to work, but no longer work. Some people have hayfever-type symptoms all year around, which is called perennial allergic rhinitis. For them, using those medications in long terms might not be a good option. Any other solutions?
Acupuncture is one of the none-drug interventions that have been shown to be effective for hayfever, and is now in the Guidelines for treating hayfever.
In the last 20 years, researches at RMIT University, Melbourne, Australia, have conducted a few randomised and controlled trials and found acupuncture was better than sham acupuncture, or fake acupuncture, for seasonal and as well as perennial hayfever.
In the hayfever season, weekly acupuncture treatments at our Geelong clinic for six weeks are needed. For those who do not like acupuncture, needle-free acupuncture can be used to stimulating therapeutic body point.
At Geelong Chinese Medicine Clinic, we will apply seeds or beads to certain areas of your ears. This is called auricular acupressure. It is “take away” treatment to sustain the effect of acupuncture. Chinese herbal medicine is also commonly prescribed for hayfever. The outcome of the combined therapies is often very good.
From a Chinese medicine view, hayfever is due to that body’s defence system being weak. Depending on your presentations, there are at least three different types of weak defence system. Treatments need to be provided accordingly to strength those systems to moderate the allergic reaction. It is also advisable to have a few treatments during non-hayfever season to prevent hayfever.
Please check our previous blog on how to reduce contact with allergens.
Spring is fast approaching and with the changing of the seasons comes an increase of pollen in the environment, which means a lot of people with allergies are going to be reaching for a box of tissues.
Allergic rhinitis (commonly known as hay fever) affects around 18% of people (children and adults) in Australia. It is caused by the nose and/or eyes coming into contact with environmental allergens, such as pollens, dust mite, moulds and animal hair.
While complete avoidance of pollen is impractical there is still a lot you can do to minimise exposure to these allergens. These range from simple measures taken around the house to changing routines. This article will focus on the simple tips for reducing pollen exposure. Other articles will focus on the treatments that usually accompany these measures.
Forewarned
Protect your home
Going outdoors
When possible avoid going outside, especially on windy days and during the early morning hours, when pollen counts are highest.
Coming home
As soon as you arrive home – even if you’ve just been in the backyard:
References:
https://www.allergy.org.au/patients/allergic-rhinitis-hay-fever-and-sinusitis/pollen-allergy
https://www.betterhealth.vic.gov.au/health/ConditionsAndTreatments/hay-fever
60 to 80% of patients who visit a primary health practitioner have some forms of pain. Dr Zheng says “Pain is a common yet complex symptom, and can affect one’s life profoundly. Pain sufferers often feel irritable, have low energy and insomnia, and can suffer from functional impairment. I believe pain and the sufferer should be understood and managed as a whole, and a combination of various therapies often achieves better therapeutic results than one particular therapy does.”
For more information, please see http://healthtimes.com.au/hub/pain-management/44/research/kk1/acupuncture-for-pain-management/1581/.